The COVID-19 pandemic has changed life for many people. Individuals with mental health conditions have been affected by the inability to interact with family and friends, which could trigger episodes and risk-taking behavior.
Individuals with bipolar disorder may be facing difficult conditions, but these challenges don’t define them. They can find compassionate, effective assistance.
What Is Bipolar Disorder?
Formerly called manic depression or manic-depressive disorder, bipolar disorder is a mental disorder that can cause shifts in mood, activity levels, concentration, energy, and the ability to complete everyday tasks.
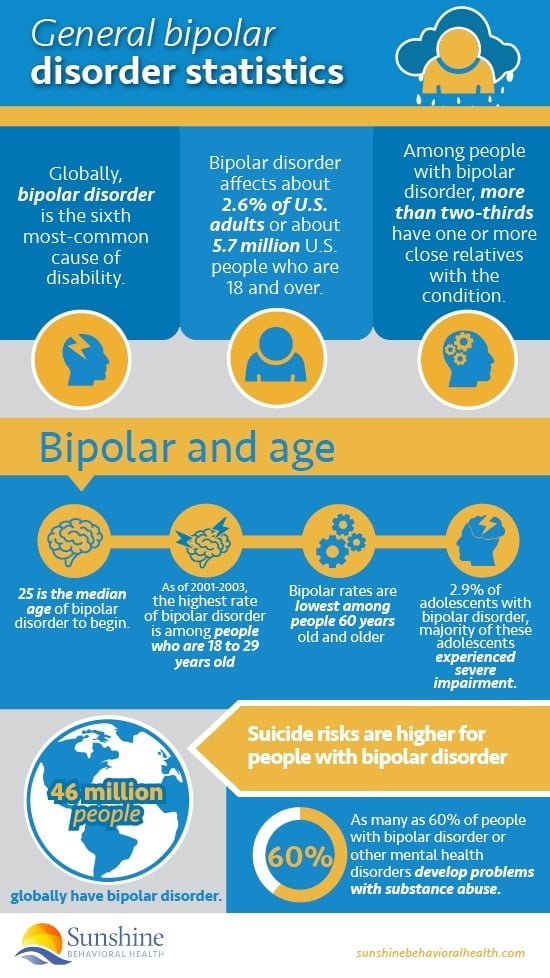
It’s a common condition. About 46 million people in the world are affected by bipolar disorder.
There are three different types of bipolar disorder that all have distinct changes in activity levels and mood shifts that can include extreme energy, profound sadness, or less severe states.
Bipolar I Disorder
With this type of bipolar disorder, manic episodes or symptoms are severe and last at least seven days. In many cases, the person is hospitalized.
Bouts of depression can also occur, lasting at least two weeks. It is also quite possible for manic symptoms and symptoms of depression to occur at the same time.
Bipolar II Disorder
Individuals with this type of bipolar disorder have patterns of both depressive and hypomanic episodes. Hypomanic behavior is behavior that is more manic than usual but not the type of full-blown mania seen in bipolar I disorder.
Cyclothymic Disorder, or Cyclothymia
People with cyclothymic disorder or cyclothymia have periods of both hypomanic and depressive symptoms that last for at least two years (one year in adolescents and children). The symptoms associated with this type of bipolar disorder do not typically meet the standards of hypomanic or depressive episodes.
There are times when someone experiences symptoms of bipolar disorder that do not correlate with any of the three categories listed above.
According to the Diagnostic and Statistical Manual of Mental Disorders (5th ed.), these conditions are categorized as “other specified bipolar and related disorders.”
Diagnosing Bipolar Disorder
In order to fully utilize the resources available for bipolar disorder, it’s important to understand how to diagnose and treat this illness. One of the first steps is speaking with a physician to undergo a series of tests and a physical exam. A mental health evaluation may be part of this process or the individual may be referred to a psychiatrist or psychologist.
A person’s symptoms, personal history and experiences, and family history can also play a role in a diagnosis. Knowing how to speak to a health care provider is also key. Here are a few tips:
Talk with health care providers
Bringing up health care concerns and feelings is important. People with mental disorders can be susceptible to other mental and physical conditions.
Speaking with providers who can refer people to specialized mental health specialists can make a significant difference.
Prepare for your visit
As helpful as appointments are, people have only limited time with their physicians, psychiatrists, or psychologists. Writing down questions and notes ahead of time could make it easier once people are in the room.
What do people want to discuss? Do they have medications? They could discuss any over-the-counter drugs, vitamins, and any supplements that they’re using.
Making notes beforehand about one’s family history can help in later discussions with a health care provider. This information can help them know and understand whether there are any underlying conditions that contribute to their patients’ bipolar disorder.
Consider bringing a friend or relative
Bringing a relative or friend to appointments can help people take detailed notes. This supportive presence can make sure health care providers cover everything the patients want to know.
Having someone else at the appointment can also assist in asking questions the individuals may have missed or remembering information the individuals may have forgotten.
Be honest about what’s happening
Clear communication is key when speaking with a health care provider. What people discuss is usually confidential in nature and cannot be shared with others.
From the very beginning, it’s important that individuals fully describe their internal and external symptoms. The more detail they give, the more accurate diagnoses health care providers can give.
If there have been any major changes or stressors that trigger symptoms, individuals should share them.
Symptoms that may be of concern include:
- Ongoing mood that is sad, “empty,” or anxious
- Pessimistic feelings, hopelessness, or helplessness
- Irritability
- Feelings of worthlessness or guilt
- Decreased pleasure or interest in activities or hobbies
- Fatigue or reduced energy
- Slow speech or movements
- Inability to sit still, feelings of restlessness
- Concentration, memory, or decision-making problems
- Sleep problems: problems sleeping, oversleeping, or awakening early
- Changes in weight and appetite
- Suicidal thoughts, suicide attempts
- Pain or aches, headaches, cramps, or digestive problems that don’t have a clear physical cause and don’t respond to treatment
 Ask questions
Ask questions
If there are any pressing questions or doubts about the diagnosis or treatment plan, patients are free to ask for more details. If there are any concerns, getting them out of the way in the beginning can help alleviate and prevent uncomfortable situations.
In some cases, it may be better to obtain a second opinion or use another health care provider. The goal is to make sure the diagnosis and treatment is compatible with the individual to attain the best results.
Bipolar disorder cannot be prevented but it can be treated. Knowing the early warning signs and seeking assistance can help regulate moods and monitor medications and other treatments.
In addition to medication and therapy, other interventions may also be helpful complements to treatment. Avoiding caffeine, alcohol, sugar, salt, and foods with high-fat content might help alleviate imbalances and triggers, for example.
Co-Occurring Disorders
Co-occurring disorders may accompany bipolar disorder, which can make treating all the conditions more challenging.
If someone has bipolar disorder with another mental or physical health challenge, it could lead to a condition known as a dual diagnosis.
Dual diagnoses sometimes cause individuals with bipolar disorder to be misdiagnosed. In fact, 7 in 10 people with bipolar disorder are misdiagnosed at least once. When people with bipolar disorder use drugs for nonmedical purposes, the effects can mimic mania.
In addition to addiction, people with bipolar disorder could have a dual diagnosis if they also have post-traumatic stress disorder (PTSD), attention-deficit/hyperactivity disorder (ADHD), physical distress in the form of migraines, heart disease, and thyroid disease, and diabetes.
Addiction and bipolar disorder can be particularly tricky. Some people with bipolar disorder might use alcohol or drugs to cope with their condition. Oftentimes this can lead to a drug abuse depression.
When people use alcohol or drugs, or when they withdraw from these substances, they might become agitated or depressed. This could make it difficult to determine if substances, substance withdrawal, bipolar condition, or other mental conditions are causing changes in moods and behaviors.
Both bipolar disorder and addiction must be treated at the same time. If only one is treated and the other is not, the treatment will be ineffective. But when bipolar disorder is correctly addressed, it can reduce the craving for harmful substances.
It appears that there are certain factors that may trigger the development of both disorders, including genetics, biology, or the environment. Furthermore, it can also be associated with other addiction personality disorders. There are also different options that can treat them, including medications and therapy.
Bipolar Disorder Resources
Resources for bipolar disorder information and treatment can help children and adults thrive:
American Academy of Child and Adolescent Psychiatry
The American Academy of Child and Adolescent Psychiatry (AACAP) is a leading nonprofit organization of physicians and other mental health professionals who help teens, children and families affected by behavioral, mental, or developmental problems.
It offers an online tool to help people find psychiatrists for children and adolescents.
American Psychiatric Association
Psychiatrists in the American Psychiatric Association aim to provide treatment and compassion for people who have mental and behavioral disorders, substance use disorder issues, and intellectual disabilities.
Its site explains what psychiatry is and offers people help in finding psychiatrists.
American Psychological Association
A huge number of psychologists belong to the American Psychological Association.
Visitors to its website can find many resources, such as hotlines, other contact information for crisis situations, and tools for finding psychologists.
American Society for Clinical Psychopharmacology (ASCP)
The American Society for Clinical Psychopharmacology (ASCP) is an organization of psychiatrists and other physicians as well as doctoral-level mental health researchers who study psychopharmacology across the country.
By logging onto the organization’s website, visitors can find a psychopharmacologist as well as other helpful information about psychopharmacology.
Depression and Bipolar Support Alliance (DBSA)
A national organization, the Depression and Bipolar Support Alliance supports people who have depression and bipolar mood disorders.
If people want to find online support groups, they can find them by using the DBSA site. Parents whose children have pediatric mood disorders can also visit the site for assistance.
International Bipolar Foundation
For people who want to know more about bipolar disorder and what to do if they’ve been diagnosed with it, this organization can be helpful.
Its site features assessment tests to help people determine if they have the condition, information about bipolar disorder, educational videos, stories from people with bipolar condition, and treatment resources.
National Alliance on Mental Illness (NAMI)
The National Alliance on Mental Illness (NAMI) supports and educates the general public about mental disorders to improve their quality of life.
Resources such as NAMI’s Help for Mental Illnesses page can help people during tough times.
Substance Use Disorder and Mental Health Services Administration
Part of the U.S. Department of Health and Human Services, the Substance Use Disorder and Mental Health Services Administration (SAMHSA) is a government resource for finding information and treatment resources for mental illness.
People can use SAMHSA’s treatment locators to find assistance for behavioral health, substance use disorder, early serious mental illnesses, and other issues.
Other Bipolar Resources
- Bipolar disorder fact sheet, Treatment Advocacy Center
- Bipolar disorder statistics – Depression and Bipolar Support Alliance
- Comorbid Medical Illness in Bipolar Disorder – article in the British Journal of Psychiatry
- Epidemiology and Risk Factors for Bipolar Disorder – article in Therapeutic Advances in Psychopharmacology
- Overview of bipolar disorder – National Institute of Mental Health
Sources
Medical disclaimer:
Sunshine Behavioral Health strives to help people who are facing substance abuse, addiction, mental health disorders, or a combination of these conditions. It does this by providing compassionate care and evidence-based content that addresses health, treatment, and recovery.
Licensed medical professionals review material we publish on our site. The material is not a substitute for qualified medical diagnoses, treatment, or advice. It should not be used to replace the suggestions of your personal physician or other health care professionals.






