PTSD from watching a loved one overdose can have debilitating effects on a person’s life and ignoring these effects will only make a bad situation worse. PTSD resources are there to help you work through painful memories, gain relief from feelings of anxiety and depression, and live a happy, productive life.
PTSD or post-traumatic stress disorder can have debilitating effects on a person’s quality of life and ability to function. Not unlike other mental health problems, the effects of post-traumatic stress disorder can vary widely depending on the person as well as on the type of event that triggered the condition. Not surprisingly, PTSD from watching a loved one overdose can leave affected individuals feeling vulnerable and empty long after their loved one passed.
Substance use disorder and addiction have long been at epidemic proportions within the United States and overdose rates have, likewise, increased accordingly. Incidentally, the risk of developing substance problems increases considerably for individuals who’ve developed PTSD from watching a loved one die. The good news is there are a host of PTSD resources available to help you heal from the effects of loss and live a happy, productive life.
What Is PTSD and What Causes It?
Traumatic experiences can have a way of “short-circuiting” the brain’s chemical and electrical makeup, creating lasting impressions that affect the way you see and experience the world around you. Trauma triggers the body’s fight-or-flight system, setting off a barrage of chemical reactions that place your body’s systems on high alert. Adrenaline levels increase, your heart beats faster, breathing rates speed up, and the body’s muscles contract.
With traumatic experiences, these physical reactions can have lasting effects on your perceptions, as well as on how you think and react to everyday events. This is how post-traumatic stress disorder or PTSD works. Not everyone develops PTSD after experiencing a trauma, however, people diagnosed with this condition have all been traumatized in one form or another.
Here are the types of experiences that can cause PTSD:
- Natural disasters, such as hurricanes or earthquakes
- Acts of terror, such as a bomb explosion
- Combat experiences, such as in war
- Rape
- Repeated exposure to violence, such as what police officers experience
- Learning about or witnessing the death of a loved one
- Physical, sexual, or emotional abuse
- Life-threatening experiences, such as car accidents and plane crashes
In effect, PTSD from seeing a loved one overdose can impact a person’s ability to function in daily life on many levels. Much like depression and anxiety-based problems, post-traumatic stress disorder can severely impact your ability to cope with situations that would normally be manageable. For these reasons, it’s important to take this condition seriously and seek professional help if you suspect you or someone you know may be affected.
Addiction’s Effects on the Family
While PTSD from watching a loved one overdose can be overwhelming, just living with someone who struggles with a severe addiction can be traumatic, in and of itself. The effects of substance use disorder not only impact the person who abuses drugs or alcohol but also the people that live with him or her. Each family member is affected differently, and often, in harmful ways.
Emotional distress, money problems, damaged relationships, and even violence are all common off-shoots of addiction and can easily become the norm in a household. Under these conditions, if PTSD hasn’t already affected one or more family members, developing PTSD from watching a loved one die from overdosing is all but guaranteed.
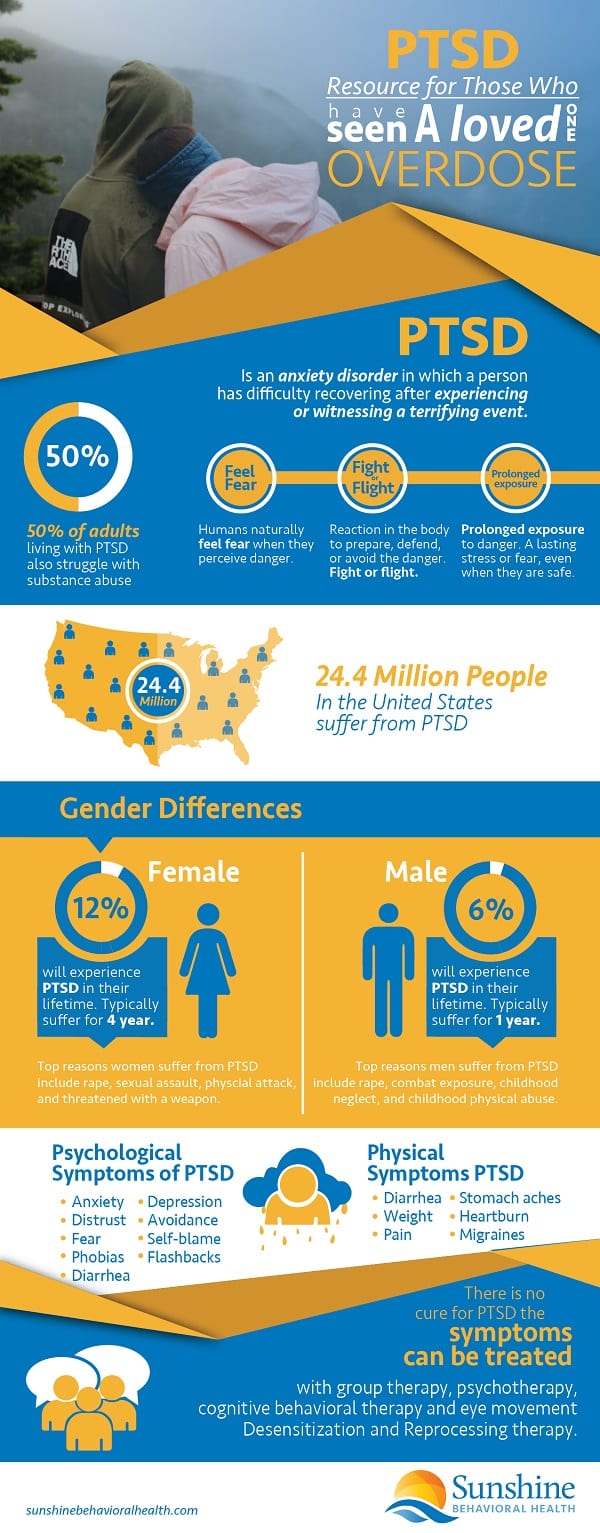
Rates of PTSD in the United States
- PTSD affects people of all ages, races, nationalities, and cultures
- Women are twice as likely to develop PTSD compared to men
- An estimated 3.5 percent of American adults have been diagnosed with post-traumatic stress disorder
- On average, one out of every 11 Americans will be diagnosed with PTSD in their lifetime
- African Americans, Latin Americans, and Native Americans all experience disproportionately higher rates of PTSD than European-Americans
Symptoms of PTSD
The effects of PTSD from watching a loved one overdose can vary from person to person but there are a few common characteristics:
- Symptoms tend to develop within three months after the traumatic event
- Symptoms persist for longer than one month
- The symptoms experienced are severe enough to impair a person’s ability to carry out the affairs of everyday life, such as work, maintaining relationships, and maintaining a household
PTSD symptom duration can vary with some people recovering within six months while others may experience continued effects for a year or longer. Also, it’s not uncommon for someone to have co-occurring mental health problems along with post-traumatic stress disorder, such as depression, anxiety-based disorders, or substance use disorder issues. This means the effects of PTSD and traumatic grief can cause other problems to develop. In like manner, someone who’s already struggling with mental health issues may be more susceptible to developing PTSD.
Overall, symptoms of PTSD fall into four main categories:
Avoidance-Based Symptoms
- Avoiding people, places, or events that remind you of the trauma
- Making changes to your normal routine to avoid reminders of the trauma
- Avoiding thoughts or feelings related to the trauma
Arousal-Based Symptoms
- Always feeling on alert or hypervigilant
- Problems sleeping
- Angry outbursts
- Being easily startled
- Taking unnecessary risks
Cognitive and Mood-Based Symptoms
- Low self-esteem
- Feeling detached from reality; like you’re observing it from the outside
- Feeling emotionally numb much of the time
- Difficulty recalling or remembering the trauma
- Problems concentrating
Re-Experiencing Symptoms
- Recurring and intrusive memories of the trauma
- Nightmares
- Flashbacks
- Panic episodes
Risk Factors for Developing PTSD After the Unexpected Death of a Loved One
A 2018 multi-study analysis conducted by the World Health Organization compared the results from 78,023 participants from several high and middle-income countries to determine which risk factors increased the likelihood of developing PTSD after the unexpected death of a loved one. The overall results from the study showed an estimated 5.2 percent of participants developed PTSD after the death of a loved one.
More than anything else, the type of relationship participants had with the deceased was the strongest predictor for developing PTSD. Here are a few things the researchers uncovered:
- Participants who lost a son or daughter were 8.7 times more likely to develop post-traumatic stress disorder
- Participants who lost a spouse were 9.6 times more likely to develop PTSD
- Participants with a history of trauma were 2.6 times more likely to develop PTSD
- Participants brought up in dysfunctional households (e.g. an alcoholic parent, a mentally ill parent, or sexual abuse) were three times more likely to develop PTSD
The results of this study address PTSD risk factors in cases of unexpected death. While an unexpected death from drug overdose is traumatizing, witnessing a death firsthand increases the degree of trauma, exponentially. Under these conditions, the risk of developing PTSD from watching a loved one die from overdosing increases, as well.
PTSD Treatment Options and Considerations
 When left untreated, PTSD and traumatic grief can have lasting effects on a person’s ability to manage daily life. Since post-traumatic stress disorder stems from a psychological and a physical component, both therapy and medication treatments have proven effective at alleviating PTSD symptoms. Traditional treatment approaches tend to lean towards therapy as a first step in the treatment process. If a person exhibits more severe symptoms, such as panic attacks, clinical depression, or anxiety, medication treatments may be used along with therapy.
When left untreated, PTSD and traumatic grief can have lasting effects on a person’s ability to manage daily life. Since post-traumatic stress disorder stems from a psychological and a physical component, both therapy and medication treatments have proven effective at alleviating PTSD symptoms. Traditional treatment approaches tend to lean towards therapy as a first step in the treatment process. If a person exhibits more severe symptoms, such as panic attacks, clinical depression, or anxiety, medication treatments may be used along with therapy.
Here’s a breakdown of the different treatment approaches used to help people overcome the effects of PTSD:
Therapy-Based Treatment Approaches
Like other forms of post-traumatic stress disorder, PTSD from watching a loved one die from overdosing warps the way a person’s brain thinks and processes emotions. In effect, PTSD sufferers have lost a fundamental sense of safety and security, and this change is reflected in how they interact with the world around them. Therapy-based treatment approaches are designed to help you work through trauma-related emotions and memories while helping you develop healthy ways of coping and managing daily stressors and triggers.
Here are three of the most commonly used therapies:
Cognitive-Behavioral Therapy
Cognitive-behavioral approaches focus on helping patients identify the faulty thinking and belief systems that developed as a result of the trauma, such as “I’m not safe,” or “love leads to pain.” From there, patients learn to replace destructive patterns of thinking with healthy ways of seeing the world around them. Since how a person thinks determines how they feel at any given point in time, progress made in correcting faulty thinking naturally helps in reducing PTSD symptom severity.
Exposure-Based Therapy
For some people, symptoms brought on by PTSD from watching a loved one die develop out of distressing, visual memories that imprint on the brain during the trauma. This is especially true for individuals who experience avoidance-based symptoms. Exposure-based therapy involves gradually exposing patients to things that trigger trauma-related fears. Over the course of 12 or more sessions, the emotional response created by the trauma becomes extinguished. In this way, patients are able to overcome trauma-related fears.
Coping Skills Therapy
Coping skills therapy uses a wide range of techniques to help patients better manage feelings of anxiety and destructive thinking patterns in their daily lives. Techniques commonly used with this approach include:
- Muscle relaxation
- Biofeedback
- Breathing techniques
- Relaxation training
- Role-playing
- Learning about PTSD and how it plays out in their daily thoughts and behaviors
Medication-Based Treatments
Severe PTSD symptoms, like panic attacks or clinical depression, can be overwhelming to the point where little to no progress can be made with therapy alone. When this is the case, medication-based treatments can help provide relief from distressing symptoms while also allowing patients to better engage with the therapy process. Otherwise, medications should not be used as the only treatment for PTSD.
Medications commonly used as PTSD treatments include barbiturates, sedatives, and antidepressants. Barbiturates work well at relieving anxiety-based symptoms, however, they should only be used on a short-term basis because of their addictive properties. Likewise, sedatives also provide relief from anxiety but are highly addictive. On the other hand, antidepressants can be used to treat both depression and feelings of anxiety. And since they have little to no potential for addiction, antidepressants can be used on an ongoing basis.
PTSD and Substance Use Disorder …Something to Consider
As helpful as therapy and medication treatments can be, if you’re struggling with a substance use disorder problem, no amount of PTSD treatment will help you get to the roots of the problem. Addictive substances, like drugs and alcohol, act as escape routes that take you farther and farther away from the issues that must be dealt with in order for healing to take place.
If you find yourself, needing a drink to take the edge off or needing to pop a few pills to face the day, these are red flags. When emotional pain goes unprocessed, it tends to come out in destructive ways, namely drinking and doing drugs. So if you suspect a drug or alcohol problem may be present or you see a habit taking shape, strongly consider getting drug rehab help. If you or someone you know experiences symptoms of PTSD and traumatic grief, the Anxiety and Depression Association of America or ADAA offers a range of helpful resources. First founded in 1979, the ADAA operates as an international nonprofit organization that’s dedicated to helping individuals heal and recover from the effects of depression, anxiety, PTSD, and a range of other co-occurring disorders. The Anxiety and Depression Association of America offers free resources and support. Here are a few to consider: The people who put their lives on the line to protect our country sacrifice their physical and emotional well-being in the process. Likewise, their families also go through experiences that the average American family doesn’t. Rates of post-traumatic stress disorder among combat veterans range from 11 to 15 percent depending on the era in which they served. On top of that, two out of every 10 service members with PTSD also struggles with substance use disorder. After all these families go through, living with PTSD from watching a loved one die from overdosing can be too much to bear. For these reasons, the PTSD Foundation of America is there to help veterans and their families overcome the effects of PTSD in their lives. This nonprofit organization offers many resources, including: Mental health and substance use disorder disorders tend to go hand-in-hand. As harmful as drug abuse (and alcohol) can be, they offer easy fixes when feelings of overwhelming anxiety or depression take hold. The Substance Use Disorder and Mental Health Services Administration or SAMHSA runs a national hotline for anyone struggling with mental health problems or substance use disorder issues. This is a 24-hour, 7-days a week free service that takes calls year-round. Operators can help you find resources in your area, including: My PTSD Forum is an active network made up of people affected by post-traumatic stress disorder. My PTSD Forum places a heavy emphasis on the importance of confronting denial and being honest about what you’re experiencing and what you’re going through. This forum also houses a reservoir of information on a range of topics related to PTSD, including: Healthful Chat, another peer-support network, offers a venue of support platforms that address not only PTSD but also depression, anxiety, ADHD, cancer, HIV, and other conditions. This resource gives you a choice between chat rooms, forums and social networks within each of their support platforms. Members of Healthful Chat come together from all over the world, seeking support and offering support to one another. Here Are a Few More Resources, to Check Out – Turn2Me, Adult Support Groups American Psychiatric Nurses Association, Information Resources and Resources for Veterans and Their Families National Center for PTSD, Veterans’ Resources Mental Health America, Self-Help Screening Tools Anxiety and Depression Association of America, Mental Health Apps
PTSD Resources for Those Who Have Seen a Loved One Overdose
Anxiety and Depression Association of America
PTSD Foundation of America
SAMHSA National Hotline (Call 1-800-662-HELP)
My PTSD Forum
Healthful Chat
Sources
Medical disclaimer:
Sunshine Behavioral Health strives to help people who are facing substance abuse, addiction, mental health disorders, or a combination of these conditions. It does this by providing compassionate care and evidence-based content that addresses health, treatment, and recovery.
Licensed medical professionals review material we publish on our site. The material is not a substitute for qualified medical diagnoses, treatment, or advice. It should not be used to replace the suggestions of your personal physician or other health care professionals.






