There is an underutilized and sometimes overlooked subset of the workforce that wants and needs employment. That would be people in recovery.
Some might write off individuals who have substance use disorders as people who should just focus on getting clean and staying that way, but there is data suggesting gainful employment can make a worker feel more self-sufficient and productive.
That’s where a recovery-friendly workplace can prove invaluable. Not only does it help the employee, but it can also benefit the company by building loyalty and cutting both healthcare and human resources-linked costs.
Substance Use Disorders
The American Psychiatric Association defines a substance use disorder (SUD) as both a mental illness and a complex brain disorder. It’s a persistent problem of compulsive drug-seeking behaviors. Over time it changes the brain’s reward circuitry.
Symptoms of SUD include:
- Lessened control
- Social impairment
- Use despite risks to self and others
- Tolerance and withdrawal
A SUD can be labeled mild, moderate, or severe, depending on how many of a set number of criteria are met, which are variations and extensions of the symptoms above.
Behavioral therapy and medications (when applicable) have proven highly successful in treating addiction.
Most people with a SUD relapse at least once, but that doesn’t mean they’re a lost cause. Addiction is a chronic disorder—as are diabetes and high blood pressure, both of which can be managed by addressing behaviors and physiological components—so relapse is not a sign of failure.
Considering the patient’s history and unique needs leads to better outcomes.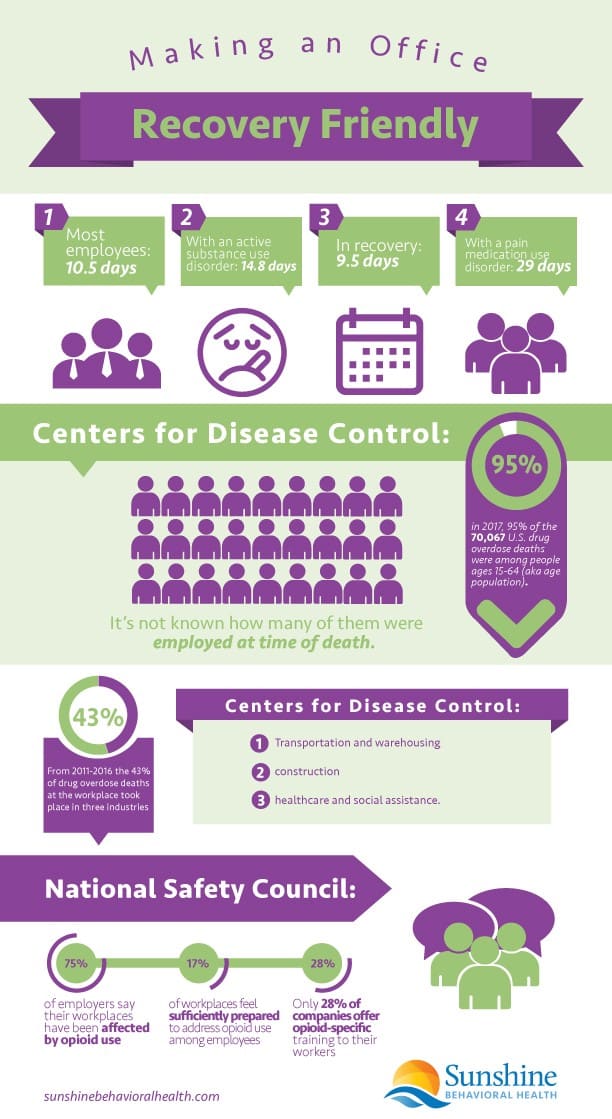
Drug Use Statistics
While the 1980s had cocaine scares, powdered and crack, the 1990s brought new synthetic opioids. Health care providers were assured these medications were safer than traditional opiates, with a low risk of addiction. Physicians were told these new opioids worked for both acute and chronic pain.
Acute or short-term pain is the type that follows an injury or surgery. Pain med dosing is usually only needed and recommended for three to five days.
Chronic pain—including palliative or end-of-life care—lasting three months or longer, affects more than 20% of adults, according to the National Safety Council (NSC). While opioids can make lives more livable, before the introduction of the new opioids, they were thought to be too addictive.
From 1999 to 2016, more and more opioids were prescribed and overdose death rates tripled. When the authorities caught on, efforts were made to rein in those prescriptions. Heroin use filled the demand, leading to more deaths starting in 2010. Then, in 2013, fentanyl—a super-opioid up to 50 times as potent as heroin—entered the equation, leading to still more drug-related deaths.
Since 1999 more than 750,000 people have died from drug overdoses. In 2018 alone, two-thirds of those deaths were opioid-related.
Drugs at Work
In 2017 more than 72,000 people died from drug overdoses. Two-thirds of those fatalities were linked to opioids.
Substance use on the job isn’t exactly rare. The NSC estimates 8.6% of working adults in the United States have a SUD, and that three-fourths of adults with SUDs are also in the workforce.
While it affects all fields, male-dominated industries like construction, mining, and manual labor have the highest rates of misuse due to higher rates of injuries. Twice as many miners (17.5%) and nearly that many construction workers (16.5%), ages 18 to 64, admitted to heavy alcohol use, compared to full-time workers (8.7%) overall.
Entertainment and food service jobs, with easier access to alcohol, also tend to have more substance users.
Many workers have prescribed opioids for injuries sustained on the job—overexertion, slips, trips, and falls—that might be managed just as well with extra recovery time or physical therapy. Many end up taking opioids in too-high doses or for longer than recommended.
The result: They risk growing dependent or overdosing. Opioids factored into more than half of off-the-job deaths.
Opiates are also problematic. Heroin was documented in 17% of workplace overdose deaths. One-third of job overdose deaths happened at companies with fewer than 10 employees, perhaps because there were fewer people ready to pick up the slack if someone gets ill or injured.
Costs of Substance Use
It’s been estimated the opioid crisis cost the US $696 billion in 2018 alone. According to the NSC, large employers spent $2.6 billion for opioid use disorders and overdoses in 2016—up from $0.4 billion in 2005.
Workers with current substance use disorders miss an average of 14.8 days each year. Those with pain medication use disorders miss an estimated 29 days every year. That’s in contrast to the 10.5-day average for most employees, or the 9.5 days for workers in recovery.
Employees under the influence tend to be:
- Less productive
- Absent more frequently
- More often ill (both long and short term)
- A danger to themselves or their co-workers (especially if operating machinery) due to reduced focus or slowed reaction time
In addition to affecting the quality of work, there are legal issues. In most states, buying or selling illegal or illicit drugs is against the law. Drinking and operating machinery, or even driving to or from work while intoxicated, can be dangerous to users and bystanders alike.
Benefits of a Recovery Friendly Workplace
There are several benefits to having a recovery friendly workplace.
Employees in recovery have:
- Lower healthcare costs
- Fewer absences
- Less likelihood of leaving an employer (which reduces hiring costs by about $4,000 per hire)
- An average of 10% fewer missed workdays
- An 8%-lower turnover rate
- Improved morale
People in recovery from opioid use disorders have said key goals are to stay busy, achieve financial self-sufficiency, and become (or return to) being productive members of society.
Reducing the stigma, offering support as needed, and being prepared in case of emergency are small tactics (in the grand scheme of things) that can yield big results.
Because heroin and fentanyl are potentially deadly because of their strength, workplaces with easy access to the overdose reversal drug naloxone or Narcan (the signs are here) can buy time for help to arrive, saving lives.
Preventing a Problem
Prevention tactics and policy changes can make a difference in keeping workers off substances or keeping them on the wagon. A safer workplace designed to reduce injuries is a good start.
A workplace culture that is supportive and open to reducing the stigma surrounding mental and substance use disorders can shed sunlight on many problems.
Being proactive by encouraging well-being—including physical, mental, emotional, social, and economic health—can prevent many issues. So can putting in place policies that give workers a chance to heal from an injury paired with better pain management options and fewer barriers to treatment.
Workplaces can offer some of that through Employee Assistance Programs (EAPs), too, so workers have access to short-term counseling or can be put in touch with support groups.
Harvard Medical School analyzed several programs and compiled five features of a recovery friendly workplace. Besides having a supportive environment, they found that having resources for counseling, support, and easily accessible treatment on-site or via telehealth could benefit the company and workers alike.
Five Key Features of a Recovery-Friendly Workplace

- Counseling options on-site. Some workers—especially manual laborers—may not be able to secure appointments during 9-to-5 office hours because it would mean lost income. Onsite counselors and telehealth resources can help to hop those hurdles.
- Peer support. Having 12-step and/or support group meetings on-site can build a stronger network. Discussing challenges, struggles, and accomplishments with fellow workers and having access to recovery coaches provides reinforcement.
- Supportive management. Relapse is not rare, so instead of firing a worker who tests positive for drug use, take it as a sign that more monitoring and support are needed. This could help reduce the stigma surrounding mental health and substance use disorders, too.
- Medication-assisted treatment (MAT). Some health insurance plans deny coverage of maintenance drugs like buprenorphine, which can help addicts better manage cravings and withdrawal while remaining productive workers. Some advocates liken that to refusing to cover insulin for diabetics.
- Onsite drug testing and telepsychiatry. Regular testing can make worksites safer (especially where heavy or sensitive equipment is used) and reveal when people may need more support. Onsite screening also means less disruption to the workday. Telepsychiatry (more common since COVID-19) means workers can receive SUD counseling from home or even the office.
The National Safety Council suggests a four-point strategy for employers to take a proactive role:
- Partner with insurance and EAP providers.
- Re-evaluate policies and testing procedures for prescription medicines.
- Invest in educating managers and employees.
- Increase and ensure that access to help and treatment is available and confidential.
Remote Workers
The COVID-19 pandemic threw the world into a tailspin, and many people have been working from home if they haven’t been furloughed or laid off.
Employed or otherwise, anxiety, trauma, stress, and depression rates rose during the pandemic. So has substance use.
The need for addiction care remains. For the remote worker who is in recovery, there are challenges.
- Programs like New Hampshire’s Recovery Friendly Workplace (RFW) Initiative have shifted gears to make sure workers in recovery have a lifeline.
- In-person visits to workplaces have stalled during shutdowns, but efforts have been made to add virtual recovery meetings and virtual coaching options.
- A clearinghouse of all available support groups and meetings makes finding help and keeping on-track easier to manage.
- Telephone check-ins and meditation apps are being made available as well.
It’s not proven ideal for all, but there are some benefits, including cutting the need to secure childcare or transportation to meetings.
The RFW Initiative also offered virtual training for employers so they can better help employees manage mental health and other hurdles they may face.
Recovery Community Organizations
Recovery community organizations (RCO) can help, too. Often independent and non-profit, they provide assistance where needed. They serve as a sort of bridge between a person’s time in rehabilitation and their long-term recovery.
RCOs are often orchestrated by people in recovery, people who are—directly or indirectly—affected by people with SUDs, or even just members of the community who want to help.
RCOs help inform the public, act as champions for those in recovery, and offer peer recovery support so those struggling realize they’re not alone.
Recovery Friendly Workplace Toolkit
The federal government and many states have resources to help employers make a workplace that is more supportive of workers in recovery. Here are several options to get started, and a couple of examples worth a look:
- Employee Assistance Programs (EAPs). EAPs can help employees struggling with personal problems, including substance use disorders. Education, assessments, referrals, and counseling are among the many EAP components available.
- National Safety Council. A free Opioids at Work Employer Toolkit with sample policies, fact sheets, videos, posters, and more.
- Recovery Friendly Workplace. This New Hampshire initiative (which has since been adopted by other areas) provides workplaces with the tools and support they need to help employees in recovery remain productive and maintain sobriety. Outreach specialists and advisors help companies develop effective policies.
- Substance Use Disorder and Mental Health Services Administration. Evidence-based practices kit to help develop Supported Employment programs to help people with mental disorders (including substance use) find work and succeed in the workplace.
Sources
Medical disclaimer:
Sunshine Behavioral Health strives to help people who are facing substance abuse, addiction, mental health disorders, or a combination of these conditions. It does this by providing compassionate care and evidence-based content that addresses health, treatment, and recovery.
Licensed medical professionals review material we publish on our site. The material is not a substitute for qualified medical diagnoses, treatment, or advice. It should not be used to replace the suggestions of your personal physician or other health care professionals.






