What Are Benzodiazepines?
Benzodiazepines or benzos are central nervous system (CNS) depressants prescribed for various psychiatric and non-psychiatric disorders, including to calm abnormal anxiety. In 2013, more than half (56%) of all benzo prescriptions were for the treatment of anxiety.
Other uses include treating alcohol withdrawal, insomnia, panic disorder, and seizures.
 Benzos largely replaced earlier drugs called barbiturates, which were too addictive and had too many dangerous side effects.
Benzos largely replaced earlier drugs called barbiturates, which were too addictive and had too many dangerous side effects.
Commonly prescribed benzodiazepines include:
- Alprazolam (Xanax)
- Lorazepam (Ativan)
- Lormetazepam (Noctamid)
- Clonazepam (Klonopin)
- Diazepam (Valium)
- Temazepam (Restoril)
- Triazolam (Halcion)
Benzos turned out to have problems, too.
What is Benzos Abuse?
Benzodiazepine medications are highly addictive. Dependence can begin within three weeks when used as prescribed.
Consequently, benzos should only be used for short-term or acute problems, not as a long-term or chronic solution.
Benzos abuse is using the drug in a way other than as prescribed, including:
- Without a prescription
- More or more often than prescribed
- Longer than prescribed.
Benzos abuse is more difficult to identify than other types of substance use disorder because it can resemble some of the conditions benzos are used to treat, including anxiety and sleep disorders.
Using benzos with alcohol, marijuana, cocaine, opioids, and other prescription drugs can be life-threatening.
Where People Get Benzos
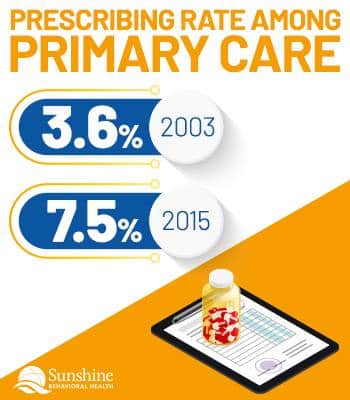
The prescribing rate of benzos by psychiatrists did not change significantly between 2003 and 2015 (from 29.6% to 30.2%). The prescribing rate among primary care physicians more than doubled, from 3.6% to 7.5%.
Between 1996 and 2013, benzos use statistics indicate that the number of benzos prescriptions filled increased for US adults, beginning at 4.1% in 1996 and increasing to 5.6% in 2013. Additionally, the amount prescribed more than doubled in that same period.
Half of all patients prescribed a benzodiazepine were diagnosed with generalized anxiety disorder. Nearly one-third took the drugs for extended periods, some reporting as long as 12 years.
Benzos prescriptions obtained through a visit to a medical provider or an emergency room more than doubled between 2003 and 2015, from 27.6 million to 62.6 million.
Roughly 80% of those who abuse benzos did not have a prescription, many obtaining the drug from friends, family, and neighbors.
Benzos Use and Addiction Rates and Numbers
Statistics on the use and abuse of benzodiazepines and other drugs are in flux.
If the latest figures are for 2015, the rate seems on the rise; for 2019, in decline. Preliminary figures for 2020 seem to show a sharp increase again.
For example, among people aged 12 and older in the United States:
- Benzos users: 28.3 million in 2019, down from 29.7 million in 2015.
- Benzos abusers: 4.8 million in 2019, down from 5.4 million in 2015.
That may have changed in 2020. At least, Americans were three times as likely to have either an anxiety or depressive disorder in 2020 than in 2019, making them more likely to seek benzos or opioids.
According to the US Centers for Disease Control and Prevention (CDC)’s Provisional Drug Overdose Death Counts for 2020, overall drug overdose deaths were up, but it didn’t break it down by type of drug.
Why People Abuse Benzos
 The reasons most often given for abusing or misusing benzos include:
The reasons most often given for abusing or misusing benzos include:
- 5.7% – Experimentation; to see what would happen.
- 11.8% – To get high or because they were already addicted
- 46.3% – To reduce tension or stress and relax.
- 22.4% – For better quality of sleep.
Women are more likely to be long-term users of benzos and abuse lormetazepam, generally prescribed for insomnia. Men are more likely to abuse the benzo lorazepam, generally prescribed for anxiety.
According to the US Library of National Medicine, unmarried or unemployed people with less education were more likely to abuse benzos but not necessarily to develop a benzo use disorder.
Benzos and Overdoses
In 2013, 30% of all prescription drug overdose deaths involved benzos, second only to opioid-related overdose fatalities. That represented a 700% increase over 1996. The highest increases were in the 18-to-64-years-old age bracket.
In 2017, there were 11,537 overdose fatalities involving benzos. In approximately 85% of these deaths, an opioid was also involved.
Benzos and Opioids
Benzos don’t kill as many people as opioids such as fentanyl and heroin. Still, benzos can exacerbate the harm of opioids and other drugs, older adults being particularly vulnerable.
Recent trend analysis indicates that co-prescription of benzos and opioids had increased 400% between 2003 and 2015, when 26.4% of patients who were already taking benzos were prescribed opioids, too.
When combined with alcohol or opioids, side effects can include:
- Slow, shallow, inadequate breathing (hypoventilation)
- Extreme drowsiness
- A dangerously slowed heart rate
- Low blood pressure
- Fainting
- Coma.
With concurrent use of benzos and opioids, the risk of overdose increases tenfold. In 2019, 30% of all opioid overdoses involved benzodiazepines; 16% of opioid-involved overdose fatalities involved benzos.
Overdoses aren’t always fatal but often require an emergency room visit or hospital admission. By 2019, 9,711 deaths involved benzodiazepines. Drug overdose deaths involving opioids were five times as large at 49,860.
In 2020, the US Food and Drug Administration updated its boxed warnings for benzodiazepines to include the risks of dangerous interactions with opioids.
Some of those interactions are due to physician co-prescriptions. Between 2003 and 2015, the number of such co-prescriptions quadrupled from 0.5% to 2.0%, though that represented a slight decline from its 2013–2014 peak.
Physician visits where both benzos and opioids were prescribed increase with the age of the client:
- Ages 18 to 44 – 4%
- Ages 45 to 64 – 13%
- Ages 65 and older – 16%.
Women were more likely than men to be prescribed both medications in general—11% vs.8%—and most age groups:
- 18 to 44 – Women, 6%; men, 3%
- 45 to 64 – No significant difference between women and men
- 65 and older – Women, 19%; men, 13%
Benzos and Age
 In 2016, roughly 12.6% of individuals aged 18 and older (30.6 million) used benzos—10.4% (25.3 million) as prescribed, 2.2% (5.3 million) abused. Of those, 82.8% used them as prescribed, 17.2% misused them. Only 1.5% had a benzodiazepine use disorder such as addiction.
In 2016, roughly 12.6% of individuals aged 18 and older (30.6 million) used benzos—10.4% (25.3 million) as prescribed, 2.2% (5.3 million) abused. Of those, 82.8% used them as prescribed, 17.2% misused them. Only 1.5% had a benzodiazepine use disorder such as addiction.
Here are the rates of benzodiazepine abuse, broken down by age group:
- 18–25 – 5% used, 5.2% abused (49% vs. 51% of the total population)
- 26–34 – 8.3% used, 3.3% abused (71.4% vs. 28.6%)
- 35–49 – 10.7% used, 1.7% abused (86.2% vs. 13.8%)
- 50–64 -12.9% used, 1.4% abused (90.3% vs. 9.7%)
- 65 and older – 12.3% used, 0.6% abused (95.6% vs. 4.4%)
Pediatric Benzos Use
There are very few stats about benzos use by youths age 12 or younger; however, there has been an increase in the rate and severity of reported pediatric benzos exposure.
In a 2017 article, PRNewswire stated that more than 130,000 children, including 39,000 infants and toddlers, had been prescribed benzos.
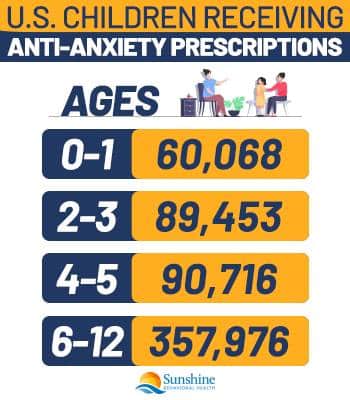
In 2020, the number of U.S. children, aged 12 or younger, receiving anti-anxiety prescriptions (including but not limited to benzodiazepines) was nearly 600,000, including:
- Ages 0-1 – 60,068
- Ages 2-3 – 89,453
- Ages 4-5 – 90,716
- Ages 6-12 – 357,976
For children younger than 2, there has been a 300% increase since 2003.
Teen Benzos Use
Teens who struggle with life stressors were prescribed benzos or other anti-anxiety drugs—571,210 individuals aged 13 to 17 in 2020. However, benzos are highly addictive, and their use may lead to abuse.
Some teens take more than prescribed. Others obtain pills from family members and friends. Some mix benzos with alcohol and other prescription or recreational drugs.
Benzos and Older Adults
Benzodiazepine use doesn’t have to be abuse to cause health problems, especially among older users.
Geriatric experts advise people aged 55 and older to avoid benzos, at least for anxiety and insomnia, because they have greater sensitivity to benzos’ effects and more difficulty metabolizing them.
Benzodiazepine use in older people can cause:
- Dizziness, leading to falls and fractures,
- Drowsiness and fatigue, leading to auto accidents.
- Negative effect on memory and other cognitive functions
Although seniors aged 65 and older had the lowest abuse of benzos, individuals aged 50 and older were more likely to take benzos more frequently than prescribed, typically using it to assist with sleep difficulties. Ironically, long-term use of benzos can worsen insomnia.
Likewise, even though physicians prescribe benzos for anxiety, benzos usage causes or increases irritability in some older adults.
Earlier concerns that benzos use could lead to Alzheimer’s (or other forms of dementia) have not been confirmed. More recent studies and surveys have found no causative effects for dementia, possibly even a small protective effect against it.
Benzos may still be appropriate for seizure disorders, some sleep behavior disorders, withdrawal from benzodiazepine or ethyl alcohol dependence, severe anxiety disorders, and as a surgical anesthetic.
Benzos Use by Ethnicity
Whites are more likely to receive a benzos prescription and be diagnosed with dependence than Asians, Hispanics, and Blacks. That discrepancy gives non-Whites some level of protection against benzos use disorder.
The percentage of Americans by ethnicity, aged 12 or older, who used benzos in 2017 was:
- 2.3% – White
- 1.9% – Hispanic or Latino
- 1.0% – Black
- 0.7% – Asian
- 2.1% – Native Hawaii and Other Pacific Islanders (NHOPI)
- 1.5% – American Indians and Alaskan Natives
Benzos and Driving Under the Influence
 The effects of benzos are similar to alcohol. Benzos usage can cause vehicular crashes because its use often leads to drowsiness, dizziness, and impaired cognitive functioning. These effects increase when combined with alcohol, marijuana, or opioids.
The effects of benzos are similar to alcohol. Benzos usage can cause vehicular crashes because its use often leads to drowsiness, dizziness, and impaired cognitive functioning. These effects increase when combined with alcohol, marijuana, or opioids.
In 2018, a benzodiazepine became the second leading cause of DUI’s in Alabama, falling only behind alcohol. For the third consecutive year, 29% of DUI cases in Alabama were due to alprazolam (Xanax), which remains toxic much longer than other benzos. Marijuana dropped to third with 23%.
There is no legal limit for benzos, however. An individual may face charges of DUI if any amount of the drug is present in the urine or blood.
Benzos Treatment and Recovery
Because benzos can be highly addictive, a physical dependence can happen even with a short treatment period of therapeutic doses. Once someone is physically dependent, stopping benzo use may cause withdrawal symptoms, from extremely mild to life-threatening.
Another study found that of benzo users who tried to quit with minimal intervention, 49% remained abstinent for at least two years, while 51% relapsed to some degree after eight months.
Sources
Medical disclaimer:
Sunshine Behavioral Health strives to help people who are facing substance abuse, addiction, mental health disorders, or a combination of these conditions. It does this by providing compassionate care and evidence-based content that addresses health, treatment, and recovery.
Licensed medical professionals review material we publish on our site. The material is not a substitute for qualified medical diagnoses, treatment, or advice. It should not be used to replace the suggestions of your personal physician or other health care professionals.







