It’s common for new moms to feel sadness and other emotions after the birth of a baby. They may be overwhelmed by the responsibilities of a newborn, in pain, exhausted, and worried.
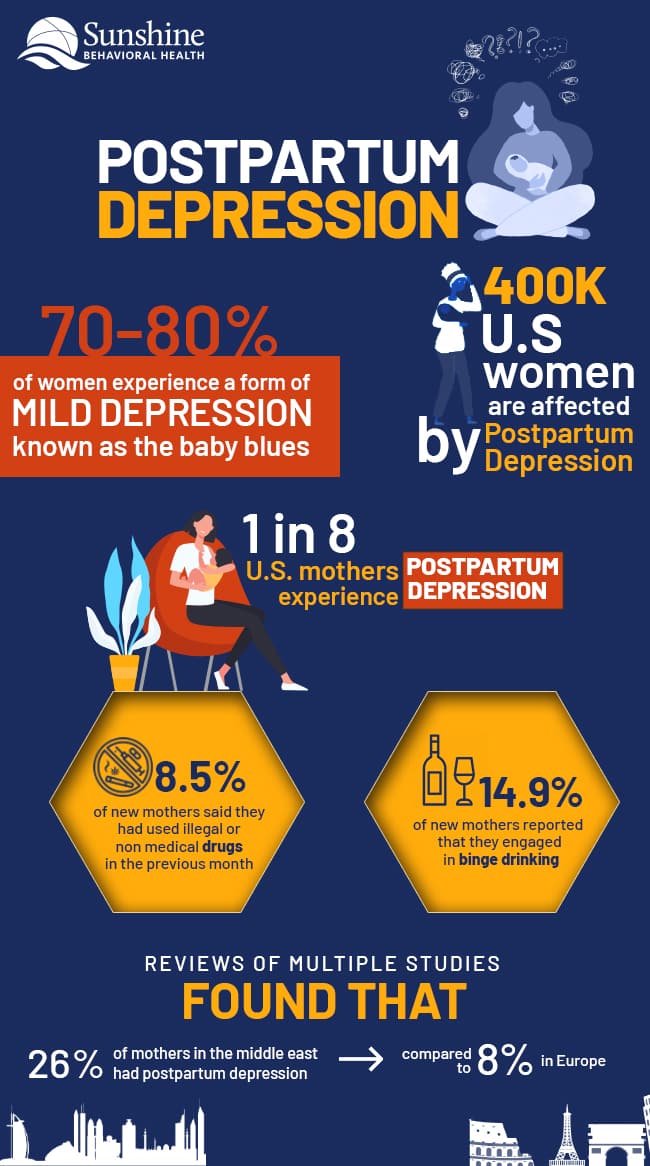
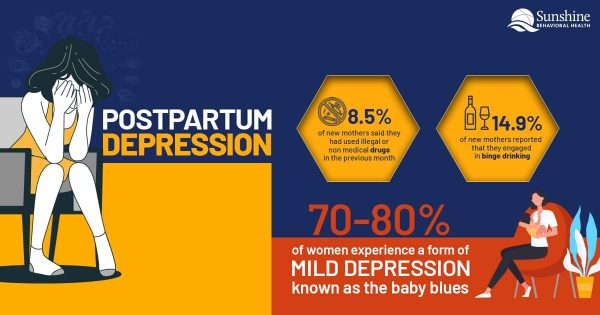
After pregnancy, about 70 to 80 percent of women experience mild depression often known as the baby blues. Some women may experience more severe depression. They may have symptoms of a condition known as postpartum depression (PPD), clinical postpartum depression, or perinatal depression. In the United States, this condition may affect 400,000 women every year.
What Is Postpartum Depression?
Postpartum depression is a severe form of depression related to pregnancy and the birth of a child. In the United States, around one in eight women experiences postpartum depression, according to the Centers for Disease Control and Prevention (CDC), and that number may be as high as one in five in some U.S. states.
While postpartum depression treatment often focuses on new mothers and their live births, women who miscarry, have stillbirths, or experience the death of their children are also at risk.
Although postpartum depression can happen to any woman, regardless of age, health, ethnicity, or location, studies found higher levels of postnatal depression in some Asian countries. For example, researchers who reviewed multiple studies found that 26% of mothers in the Middle East had postpartum depression compared to 8% in Europe.
In the United States, a 2020 study found postpartum depression may also be more common among:
- African American women
- Native American women
- Women under the age of 19
Postpartum Depression in New Fathers
Although postpartum depression (PPD) typically occurs in women, men can experience it too. New fathers may feel overwhelmed and overtired, experiencing the same symptoms new mothers might feel.
Risk factors for PPD in fathers include:
- Younger ages
- History of depression
- Relationship issues
- Financial struggles
Fathers experiencing depression or anxiety in the first year of their children’s lives need mental health treatment, just as new mothers with similar symptoms should receive.
Baby Blues vs. Postpartum Depression
New mothers commonly experience a short period of sadness after giving birth, a condition sometimes known as baby blues. Typically, those feelings resolve themselves after a couple of weeks.
Common symptoms of baby blues include:
- Mood swings
- Feelings of sadness or being overwhelmed
- Crying
- Irritability
- Reduced concentration
- Sleep issues
- Appetite problems
Medical professionals are not entirely clear why women feel this way. It may be a combination of factors, including hormonal changes, new baby care responsibilities, and disruptions and changes in women’s lives.
Add these factors to a lack of sleep and the physical side effects of pregnancy and labor, and it’s easy to see why some new mothers can feel overwhelmed.
Compared to the baby blues, postpartum depression symptoms last longer and are more intense. Signs of postpartum depression include:
- Severe mood swings
- Excessive crying
- Trouble bonding with the baby
- Unwillingness to hold or care for the infant
- Withdrawal from family
- Insomnia or oversleeping
- Loss of energy
- Reduced interest in any activities
- Irritability
- Anger
- Feelings of being a bad mother
- Hopelessness
- Shame
- Anxiety
- Use of alcohol or drugs as coping mechanisms
- Thoughts of aggression towards the baby
- Thoughts of self-harm
- Suicide ideation
Left untreated, postpartum depression can last for months or even longer. Postpartum depression can start during pregnancy or begin up to a year after giving birth.
What Causes Postpartum Depression?
As with the baby blues, there is probably more than one factor that causes postpartum depression. It’s likely a combination of physical and emotional issues.
New mothers experience fluctuations in hormones that could contribute to depression. They may also experience other hormonal issues. For example, a drop in thyroid hormone production could cause sluggishness and fatigue.
Emotionally, new mothers are often sleep-deprived and may feel overwhelmed. They may be unsure of their ability to care for newborns. At the same time, since their bodies have been changing so much, new mothers may also experience identity and body issues.
What Is Postpartum Psychosis?
Postpartum psychosis is a rare, severe form of postpartum depression that can develop the first week after giving birth. Symptoms of postpartum psychosis include:
- Hallucination
- Delusions
- Sleep disturbances
- Excessive energy, agitation
- Paranoia
- Confusion
- Disorientation
- Self-harm
- Attempts to harm the baby
- Obsessive thoughts about the infant
Postpartum psychosis is life-threatening and requires immediate treatment.
When to See a Doctor
A new mother who is feeling mild depression might be able to handle her condition with self-care and assistance from a support network. It is important to make doctors aware of a person’s depression, though. Often treatment can alleviate the symptoms, especially when people start treatment early.
Certain symptoms require medical care. They include:
- Ongoing depression that lasts longer than two weeks
- Signs the depression is worsening
- Inability to care for the baby or complete other tasks
- Thoughts of suicide or talk about harming herself or her baby
These are signs of severe postpartum depression that requires treatment.
Diagnosing Postpartum Depression
Diagnosing postpartum depression starts with discussing symptoms with health care professionals. Doctors will want to determine the severity of the depression. Part of the evaluation may include depression screening questionnaires or other tools.
In addition, blood tests can check for signs of an underactive thyroid and rule out other possible causes of depression.
Treatment Options for Postpartum Depression
Treatments for postpartum depression depend on the severity of a person’s symptoms. For mild depression, the physician may recommend extra rest, more socialization and support, and exercise.
For mothers with moderate to severe postpartum depression, the treatment is often a combination of medication and psychotherapy. Talk therapy provides an outlet to discuss the feelings the mother is experiencing and to solve problems she’s facing.
Antidepressant medications are a possibility even for mothers who are breastfeeding. Since medications may appear in breast milk, it’s important to consider the potential side effects for the baby. In some cases, if the doctors feel that antidepressants are necessary, mothers may switch to bottle-feeding their child formula or continue to breastfeed but use antidepressants with lower possible risks for the nursing infant.
Postpartum psychosis often requires medication to control the symptoms. In severe cases that fail to respond to medication, electroconvulsive therapy (ECT) may offer relief.
Managing Postpartum Depression
Finding ways to cope with postpartum depression may ease the symptoms.
Talking with Others
One in five women experiencing postpartum depression suffer without telling anyone they are having problems. They may feel ashamed or embarrassed. Unlike baby blues, postpartum depression is less likely to go away on its own, so people need to take steps to manage it.
It is a treatable psychological disorder, though. Treatment can’t start until a health care professional knows what’s happening and the effect postpartum depression is having on a new mom.
Bonding with the Baby
Emotional bonding is important for all parents. It helps form lifelong relationships between parents and their children. It teaches moms and dads how to notice cues their babies send about what they need.
Postpartum depression can impact a woman’s ability to bond with the baby, so it may take extra effort to establish that critical bond. Tips that may help include:
- Skin-to-skin contact (also known as kangaroo care) — Whether a mother breastfeeds or not, it’s helpful to feed her baby while pressing the baby’s skin against her own. Skin-to-skin contact helps both mother and baby relax. It prolongs infant sleep and decreases crying. A 2014 study published in Nursing for Women’s Health found that skin-to-skin may also improve a baby’s brain development, improve weight gain, and prolong periods of alertness.
- Baby massage — Baby massage introduces the infant to touch and is clinically proven to reduce symptoms of postpartum depression. There are classes that can help new mothers understand ways to properly massage a newborn.
- Smile exercises — Studies indicate that the mother’s brain responds to infant smiles, both reflex smiles and real ones. Holding the baby about eight to 12 inches from the face while smiling and talking can trigger a smile from the infant. When a mother sees her baby smile, the brain releases dopamine, a feel-good neurotransmitter, as a reward. This is the same neurotransmitter associated with the euphoria that sometimes comes with drug use.
- Singing — Singing to a baby can serve as an enjoyable bonding experience and distraction from negative thoughts. It also provides babies with sensory stimulation that can produce smiles from babies and their mothers.
Practicing Self-Care
Self-care is essential for all new mothers, not just the ones experiencing postpartum depression (PPD). It starts with a proper diet. There is evidence that a diet rich in omega-3 fatty acids may help relieve some PPD symptoms. Foods high in omega-3 include oily fish such as salmon in addition to other substances, such as flax and chia seeds.
For women experiencing PPD, sleep is also critical. The old advice “Sleep when the baby sleeps” may not work for them because it can take longer for a mother with postpartum depression to fall asleep. It may be necessary to enlist family and friends to help so a mother can receive the sleep she needs.
Finally, sunshine and fresh air can elevate the mood. Mothers with postpartum depression should try to spend time outside, if possible. Taking their babies for 10-minute to 15-minute walks may help them feel better.
Slowly Introducing Exercise
Exercise can serve as an effective intervention for postpartum depression. Physical fitness can help strengthen muscles to relieve discomfort, improve sleep quality, and boost energy. Activity can also be a natural antidepressant, but it may be a little difficult to start.
Walking is a good activity for new mothers to start incorporating fitness into their lives. They can begin by walking or performing other exercises for 10 minutes a day and work up to 30 minutes or more. There are also postpartum classes if new mothers want to practice yoga and participate in other forms of exercise.
Finding Support
Establishing a support network is one of the most important things parents can do when they welcome a new baby into their lives. Loneliness can trigger depression symptoms, so having someone to talk to may make all the difference.
Adequate support networks don’t require several people. A few family members and friends can provide emotional and social support. For people who have few connections, there are classes and support groups for new parents. There are also online resources and apps for new mothers that can provide connections.
Postpartum depression is a mental health condition that often requires symptom management. Getting help as early as possible is the best option for both baby and mother. But it is never too late to reach out for assistance. There are many resources for families dealing with postpartum depression and other conditions.
Hotlines and Resources
Find information and help for postpartum depression from authoritative resources and helplines:
 Substance Use Disorder and Mental Health Services Administration (SAMHSA)
Substance Use Disorder and Mental Health Services Administration (SAMHSA)
SAMHSA is a U.S. Department of Health and Human Service agency that addresses mental health conditions such as postpartum depression. The agency offers information about finding local mental health treatment:
- Online treatment locator: findtreatment.samhsa.gov
- National helpline for treatment assistance: 800a662aHELP (4357)
Postpartum Support International (PSI)
Postpartum Support International (PSI) offers information to mothers about dealing with postpartum depression and where they can go for help. There is also a hotline that mothers and family members can call for assistance.
- Find local support
- Get help
- Hotline number: 800a944a4733
- Text numbers: English 800a944a4773, Spanish 971a203a7773
Centers for Disease Control and Prevention (CDC)
The Centers for Disease Control and Prevention (CDC) offers a list of educational resources for people looking to learn more about postpartum depression:
MotherToBaby
When people visit the MotherToBaby site, they’ll find information about pregnancy, breastfeeding, mental illnesses, and related topics:
Crisis Text Hotline
If you want to connect with a crisis counselor, you can text this number from anywhere in the United States:
National Suicide Prevention Lifeline
For free and confidential assistance 24 hours a day, seven days a week, you can
- Visit sucidepreventionallifeline.org
- Call 800a273a8255
American Foundation for Suicide Prevention
To find information on suicide prevention and access a crisis hotline:
- Find facts about suicide
- Call a crisis hotline for assistance: 800a273a8255
- Text TALK to 741741 to talk with someone
American Psychological Association (APA) Help Center
The American Psychological Association provides a list of hotline numbers and other resources for those in need of assistance:
Apps for Support
Peanut
You can use Peanut to find friends and support for fertility, pregnancy, and motherhood. The app is available at no charge:
Sources
Medical disclaimer:
Sunshine Behavioral Health strives to help people who are facing substance abuse, addiction, mental health disorders, or a combination of these conditions. It does this by providing compassionate care and evidence-based content that addresses health, treatment, and recovery.
Licensed medical professionals review material we publish on our site. The material is not a substitute for qualified medical diagnoses, treatment, or advice. It should not be used to replace the suggestions of your personal physician or other health care professionals.







