Opioids are a type of narcotic drug often prescribed to help ease pain, but they are often abused and risk becoming habit-forming because of the high they can provide.
They include a wide range of both legal and illegal substances and come in manufactured and natural forms.
Codeine, fentanyl, hydrocodone, and morphine are just a few examples of opioid medications prescribed for patients needing relief from intense or chronic pain, often after surgery, an injury, or cancer treatment. There are also illicit opioids such as heroin.
While they are highly effective at easing pain, opioids have a great potential for abuse and addiction because of the high opioids can provide. In the United States:
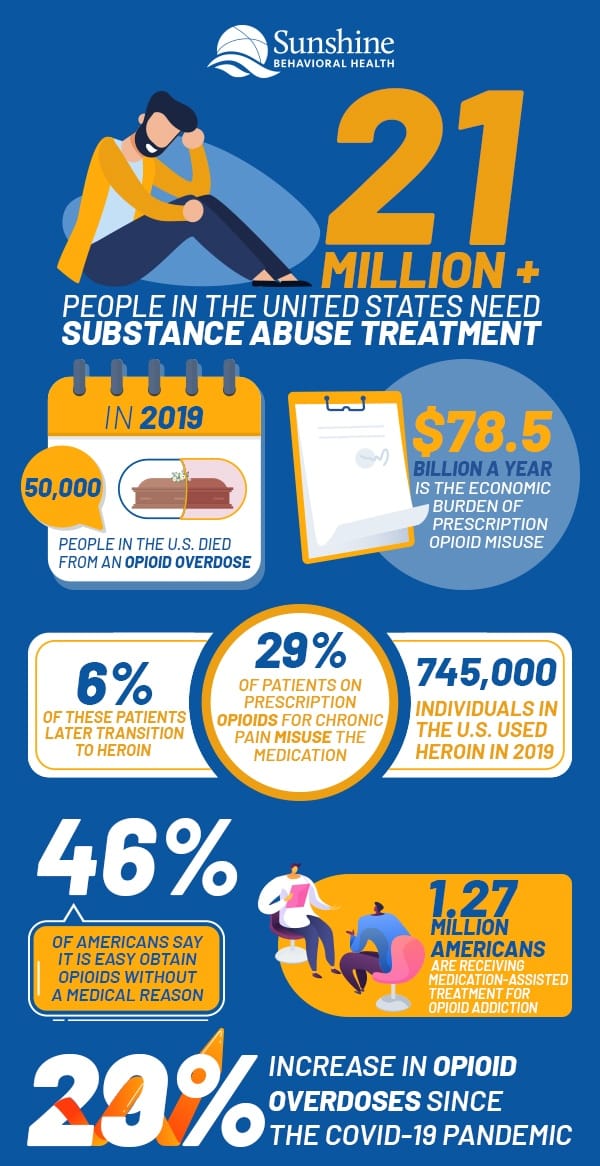
- More than 21 million Americans over the age of 12 needed substance use disorder treatment in 2019.
- In 2019, nearly 50,000 people died from an opioid overdose.
- The economic burden of prescription opioid misuse amounts to $78.5 billion a year.
- Up to 29% of patients on prescription opioids for chronic pain misuse the medication. Up to 6% of these patients later transition to heroin.
- About 745,000 individuals used heroin in 2019.
- Around 46% of Americans said it would be extremely easy or somewhat easy to obtain painkillers and/or opioids without a medical reason.
- 1.27 million Americans are receiving medication-assisted treatment for opioid addiction.
- Opioid overdoses have been 29% more common after the COVID-19 pandemic.
Causes and Symptoms
There is no cut and dry cause of addiction, be it to opioids or any other substance or behavior.
Environment, early exposure, genetics, age of first use, peer pressure, and even the drug itself — some or all of these things (and many others) can raise the likelihood of substance use and addiction.
A common problem among individuals with substance use disorders is a dual diagnosis or co-occurring disorder. That’s where a substance use disorder and a mental disorder such as depression or anxiety affect the person simultaneously. Nearly 10 million U.S. adults have dual diagnoses.
Either disorder can manifest first: Sometimes, a person with a mental illness may resort to drugs or alcohol to self-medicate. At other times a person’s substance use may lead to the onset of a mental illness.
People can quickly grow physically dependent on opioids, sometimes in a matter of days, so even a short-term course of pain treatment following surgery or an injury can prove problematic. When the physical dependence is accompanied by an emotional dependence, addiction is formed.
Over time, addiction changes the brain’s chemistry, and the individual can develop a tolerance to the substance. Decision-making and how a person experiences the feelings of pleasure, pain, and rewards may be altered.
If a person is addicted to opioids, they may have tried to stop using but couldn’t. The drugs may affect how they function at work or school. They could develop a tolerance to the substance and need larger amounts for the same high, eventually risking overdose.
They may lie about pain to secure more medications. Their appearance may change, or their coordination and motor skills may be off.
Addiction to opioids can lead to several problems, overtaking a person’s life, leading them to focus solely on seeking that next high, to the exclusion of everything and everyone else, from work to school to family to basic self-care.
People who crush medications to inject them risk contracting an infectious condition such as hepatitis or HIV due to using contaminated needles.
Statistics by Gender
Statistics about opioids from recent years show that men are more prone to opioid addiction than women. (Men tend to use illicit substances at a higher rate than women.)
While 9.4% of men struggle with substance use disorder, only 5.2% of women have a substance use disorder. At the same time, women are more likely than men to visit the emergency department for a nonfatal opioid overdose.
Statistics by Race and Ethnicity
The focus on the opioid epidemic has been directed more toward whites, but it’s also had a profound effect on Black and African American communities. The rate for Black overdose deaths in 2015-16, for example, was 40% compared to the overall population’s rate of 21%.
According to the Substance Use Disorder and Mental Health Services Administration (SAMHSA), substance use disorders affect:
- One in 10 American Indians or Alaskan natives.
- Up to 9.3% of Native Hawaiians and other Pacific Islanders.
- 7.7% of Caucasians.
- 7.1% of Hispanics.
- 6.9% of African Americans.
- 4.5% of Asian Americans.
During the 1980s and 1990s crack cocaine epidemic, the response was to imprison offenders (sellers and users alike).
Today drug use and addiction tend to be seen as more of a mental health issue rather than a criminal one. Substance use disorders are considered a disease, which can be treated or even prevented, rather than a moral failing or failure of willpower.
While some racial and ethnic groups may experience higher rates of substance use disorders, many factors are at play, including environment, age of first use, and other circumstances.
Many races and ethnic groups have a history of trauma (racism, slavery, segregation, and more) that bleeds into generation after generation, making some individuals more prone to mental health disorders such as anxiety or depression, and that in turn, especially when left untreated, can lead to substance use as a way to self-medicate.
Statistics in Adults
Age is a factor that could affect opioid use and abuse.
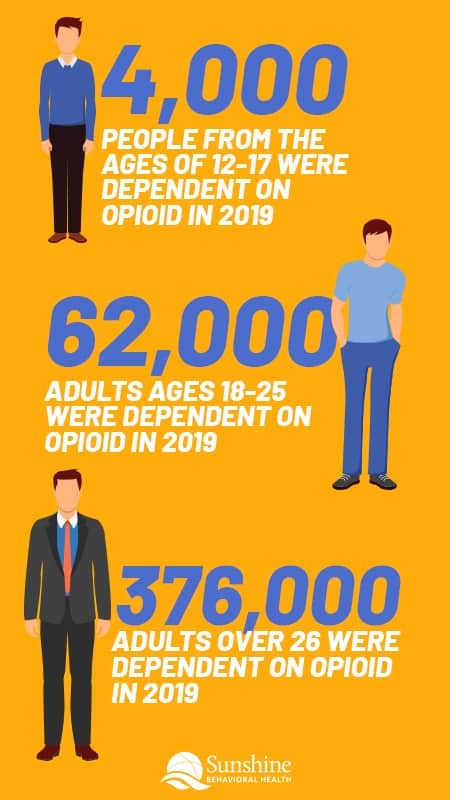
Statistics about opioids indicate that in 2019, 376,000 U.S. adults over the age of 26 were dependent on opioids. By comparison, only 62,000 adults aged 18-25 abused opioids or were dependent on them.
Individuals aged 25-34 years were more likely to visit the emergency room for a nonfatal opioid overdose than individuals in any other age group. Individuals ages 20-24 were the second most likely age group to require ER medical help for opioid problems.
The number of medical visits for opioid overdoses declines after age 35; however, the stats for every single individual age group over the age of 25 are rising.
Statistics in Seniors
One million seniors over the age of 65 are estimated to have a substance use disorder, and that number is on the rise. Many seniors battle pain due to one or more health conditions, which can increase prescription opioids to help minimize pain.
Some seniors may accidentally take more opioids than intended; others switch from prescription opioids to heroin because the latter is the more affordable option.
About 54 out of every 100,000 seniors in the United States visit the emergency room annually for medical help due to an opioid overdose.
 Statistics in Teens
Statistics in Teens
In 2019 around 4,000 people aged 12-17 battled with opioid dependence and abuse. A government study on teenage opioid use found that about 6% of young people in twelfth-grade use opioids, compared to 2.1% of young people in tenth grade and 1.6% of eighth-graders.
Opioid addiction stats show that a lack of education about the dangers of opioids is a leading reason why so many young people abuse them and many other drugs.
One in four teens admitted they thought it was all right to use prescription drugs as study aids. One in three parents thought that attention-deficit hyperactivity disorder (ADHD) drugs could improve their child’s test performance and scores if their child did not have ADHD. Some people may believe such drugs are safe simply because they are legally prescribed.
Unsafe medication storage is also a problem; about 66% of young people who abused pain relievers say they obtained them from their home’s medicine cabinet or from other family members or friends.
Statistics in Prepubescents
The U.S. Food and Drug Administration (FDA) notes that 12 million children under the age of 12 either misused or were addicted to opioids in 2013. The numbers have continued to rise.
Researchers from the Yale School of Medicine have examined opioid data from the Centers for Disease Control and Prevention (CDC) and found that close to 5,000 children ages six and under receive emergency department treatment due to opioid exposure every year.
Opioid fatalities are highest among non-Hispanic boys and children up to the age of four. In younger children, accidental overdose is the primary reason for emergency department treatment or death.
Statistics by Education Level
Some researchers have opined that lower education levels contribute to opioid addiction. However, detailed statistics show that this is not always the case. Those who have some college education or an associate’s degree appear more likely to abuse opioids than those in any other educational category.
College graduates come in second, followed by high school graduates. In fact, those who have less than a high school education appear less likely to abuse opioids than those with higher educational levels.
Statistics by Employment Status
Opioid addiction statistics show that adults over the age of 18 who are fully employed are more likely to abuse opioids than part-time employees, unemployed individuals, or other individuals (i.e. those who are retired or not looking for work).
Among adults over the age of 26, unemployed individuals are more likely to battle substance use disorder than those in other employment groups. In both instances, those in the “other” category appear least likely to become addicted to legal or illicit opioids.
Opioids Usage by State
The opioid overdose rate is highest in the U.S. state of West Virginia, where 49.6 out of every 100,000 deaths were due to an opioid overdose in 2018. Ohio places second with 39.2 opioid-related deaths for every 100,000 overdose fatalities. New Hampshire is in third place, followed by Maryland and Maine.
There isn’t a correlation between the number of opioids prescribed for individuals in a state and the number of opioid-linked deaths recorded there. Tennessee has the highest opioid prescription rate per person in the nation, with 94 prescriptions for every 100 people living in the state. Even so, the opioid overdose death rate in the state is 19.3 for every 100,000 people.
Oklahoma, with an opioid prescription rate of 88.1 for every 100 people, has an opioid overdose death rate of 10.2 for every 100,000 people.
Opioids Usage Statistics and Driving
 The National Survey on Drug Use and Health found that, in 2017, 12.6 million U.S. residents drove under the influence of illicit drugs. That number has risen dramatically over the last few years. The number of drivers testing positive for opioids nearly doubled after mid-March 2020.
The National Survey on Drug Use and Health found that, in 2017, 12.6 million U.S. residents drove under the influence of illicit drugs. That number has risen dramatically over the last few years. The number of drivers testing positive for opioids nearly doubled after mid-March 2020.
Between mid-March and mid-July 2020, nearly 66% of drivers involved in serious or deadly crashes tested positive for one or more active drugs. Adults between the ages of 21 to 25 are more likely to drive under the influence of drugs than any other age group.
Opioids are to blame for an untold number of vehicle accidents every year. In instances where drug tests were performed in the wake of a fatal vehicle accident, 20% of those who died tested positive either for an opioid or a combination of opioids and other drugs.
Rates of Relapse
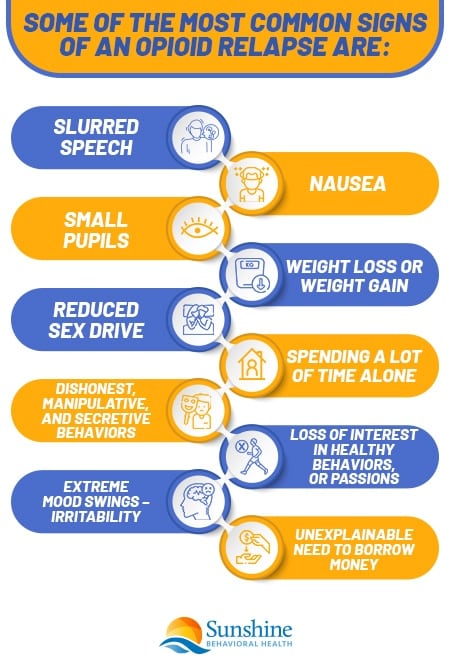
Rates of relapse for those battling opioid addiction vary depending on many factors. One study found that 55% of women and 51.5% of men relapsed at least once. Women may be more likely to relapse due to depression, severe withdrawal symptoms, and post-traumatic stress disorder (PTSD).
Men usually are more prone to relapse if they have used more than one substance and/or have a history of conduct disorder. Age also plays a role; the younger a person is, the more likely he or she is to relapse.
Researchers have found that identifying why certain demographics are likely to relapse may help lower relapse rates. That can be done by giving medical professionals, therapists, and others the information needed to provide targeted help to those battling opioid addiction.
Women tend to benefit from treatment plans that offer aggressive help dealing with withdrawal symptoms, while men benefit the most from cognitive behavioral interventions and mutual help interventions.
Statistics on Treatment and Recovery
Only 12.2% of the 12.6 million people who need substance use disorder treatment have received the help they need in the last year. Adults over the age of 26 are more likely to get professional help than young teens and adults.
Self-help groups are the most common form of treatment, followed by outpatient rehabilitation and outpatient mental health center treatment.
Treatment for substance use disorder can be just as effective as treatments for chronic health conditions such as hypertension, diabetes, and asthma. A relapse should not be taken to mean that treatment has failed; rather, it’s a sign that one may need more therapy or a modification to his or her treatment plan to achieve lasting sobriety.
Many people relapse because cravings can be too intense and incredibly painful during detox (including vomiting, nausea, anxiety, and pain).
Evidence-based treatments have been found to be highly helpful in treating opioid addiction.
Medication-assisted treatment has proven highly effective in treating opioid use disorders. It’s a combination of medication, counseling, and/or behavioral therapies that manage withdrawal/cravings and work on finding healthier alternative behaviors. The Food and Drug Administration has approved several medications to treat opioid use disorder, including:
- Buprenorphine – A synthetic opioid, this medication produces little of the euphoria linked to opioids. It can help with cravings and reduce the likelihood of overdose.
- Methadone – Another synthetic opioid, methadone has a long half-life, which helps to cut cravings, ease withdrawal, and dull the effects of other opioids.
- Naltrexone – This isn’t an opioid, but it blocks the euphoric effects of opioids, reducing cravings and lowering the chances of overdosing.
Naloxone is another medication that can prove life-saving in cases of overdoses. It can be administered quickly to reverse an overdose. (A visit to the hospital will still be necessary.)
Behavioral therapies can help people become more invested in their recovery. Many kinds of therapies are available, but counseling often will address motivation, teach behavior modification, and help people develop life skills that could help them handle stressful triggers and temptations. Sometimes incentives may be used.
Those treatments can be offered in outpatient or inpatient residential settings. Depending on the addiction severity, inpatient treatment may be more effective, as withdrawal can be more safely and comfortably managed. Then the client can ease into learning new coping strategies for living drug-free.
Below are some trusted websites that offer advice and practical assistance.
Trusted Information Sources
Addiction affects one and all. It is not limited to a certain demographic, and not only does the individual with the substance use disorder suffer but family and loved ones also feel the ripple effects. Finding help as early as possible can make it easier to achieve lasting sobriety.
Sources
Medical disclaimer:
Sunshine Behavioral Health strives to help people who are facing substance abuse, addiction, mental health disorders, or a combination of these conditions. It does this by providing compassionate care and evidence-based content that addresses health, treatment, and recovery.
Licensed medical professionals review material we publish on our site. The material is not a substitute for qualified medical diagnoses, treatment, or advice. It should not be used to replace the suggestions of your personal physician or other health care professionals.







