Many first responders who work in emergency medical services, firefighting, and police services experience mental health or substance use disorder issues. Not only are the jobs inherently stressful, but there may not always be a support system available for them. First responders experience unique challenges when dealing with mental health and substance use disorder problems, and consequently may not be willing to or able to seek conventional help.
Many mental health issues can segue into substance use disorder problems. Substance use disorder problems can also lead to stress, anxiety, depression, and other mental health problems. Thus, mental health problems and substance use disorder problems often occur at the same time and need to be treated at the same time.
Here’s an overview of how first responders may experience mental health and substance use disorder issues, what symptoms they might display, and how they can find help.
What Mental Health Issues May First Responders Experience?
Many first responders experience high-stress situations, are witnesses to violence, or work in traumatic environments. Because of this, first responders may experience issues such as anxiety, depression, or post-traumatic stress disorder (PTSD).
To perform in such conditions, first responders may not want to show their emotions or deal with their emotions. But not addressing their emotions could contribute to mental health issues that could become severe.
There are many mental health issues that first responders could experience. PTSD is one of the most common issues, along with depression, anxiety, and stress-related issues. Suicide and suicide ideation (thoughts of suicide) may be prevalent and are particularly important to address right away.
In addition to this, first responders may experience substance use disorder issues, which may be co-occurring with other disorders.
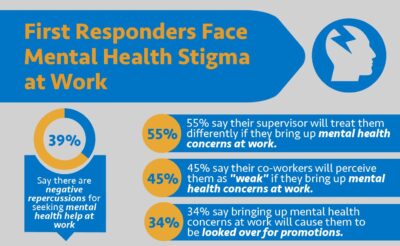
As others who have jobs in high-pressure environments, first responders may be concerned that their mental health issues could put their jobs at risk.
They may not be willing to discuss substance use disorder problems or mental health issues with their superiors to find the help they need. They might be afraid that their competence will be called into question or they might be asked to step down from their roles.
People who have mental health issues that are separate from their working environments, such as a history of depression rather than trauma-related PTSD, may equally be hesitant to reveal their issues to their superiors.
Consequently, it can be difficult for first responders who have mental health issues to open up to others, talk with their colleagues, or find help from their human resources department. They may feel that if they tell their colleagues they are suffering, their colleagues won’t trust them in intense environments.
People with mental health issues might worry that their human resources departments may be more willing to discontinue their services than allow them to find the help they need. They may feel isolated and alone because they may feel as though others don’t really understand what they’re experiencing.
There is protection available for first responders who have mental health issues or substance use disorder issues. But first responders may feel that they need an advocate on their side before they take these first steps. Connecting with advocates, resources, and first responder groups can give someone the backing they need to advocate for themselves.
Symptoms of mental health issues might include:
- Feeling irritable or frustrated much of the time.
- Experiencing depression, low energy, or sleep problems.
- Engaging in substance use disorder.
- Having thoughts of suicide (suicide ideation).
What Problems With Substance Use Disorder Could First Responders Encounter?
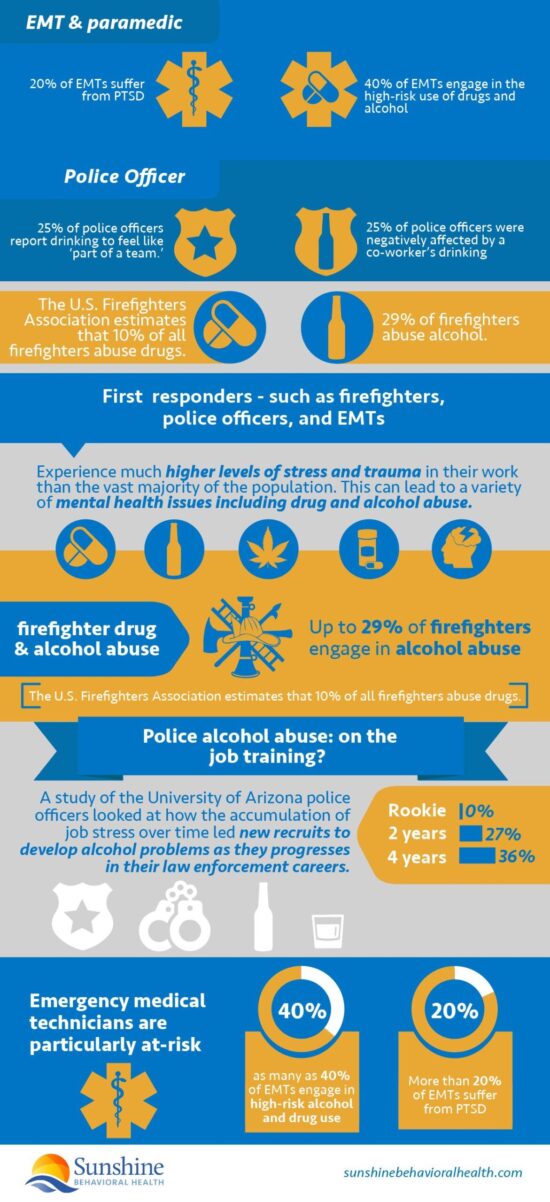
Substance use disorder issues often occur due to other problems. As an example, a first responder might experience depression, which they then treat with alcohol. For instance, police alcoholism is rampant due to this issue. Or they may experience anxiety and treat it with anxiety medications that aren’t prescribed to them.
Trauma may make it difficult for a person to sleep, so a person might become reliant on sleep medications and become addicted. Dealing with substance use disorder issues is often complex because people need to resolve the underlying conditions alongside the addictions itself.
Because first responders may not feel that they can enlist professional help, they may seek to self-medicate using substances. This can spiral into addiction, since they’ll be abusing substances not only because of their depression, but because they also require alcohol or drugs to function.
Because of the intense stress of their work, first responders may be more likely to abuse alcohol and other substances, and this may become an environmental issue. Consequently, those with substance use disorder issues may also be in high-risk environments and may be more tempted to use substances even if they are trying to reduce their usage.
First responders may also simply have a substance use disorder issue; some may have a substance use disorder issue that does not come hand-in-hand with another disorder but could be more environmental or genetic.
Finally, first responders may have physical issues that can leave them vulnerable to addiction. For instance, firefighters could have back problems that could lead to the use of pain medication, and they may then become addicted to the pain medication.
The connection between the issues can be complex. When chronic pain and substance use disorder occurs at the same time, the chronic pain also has to be addressed. Unfortunately, it may not always be possible for an individual to continue their previous job responsibilities if they are addicted to opioid pain relieving drugs or other medications.
Compounding this, the stress of a first responder’s environment can lead to chronic pain and chronic fatigue or worsen existing medical conditions.
As with mental health issues, first responders may be reluctant to let their superiors know about their substance use disorder problems. They may fear reprisal. They may fear that their work will be examined with scrutiny or that they will be removed from service.
Because of these fears, first responders may go a long time without help, and may continue to struggle. Unfortunately, their concerns may not always be unfounded, and it could lead to work-related problems if their substance use disorder is discovered.
Some symptoms of substance use disorder include:
- Being unable to go to work or go to sleep without abusing substances.
- Being unable to go a long period of time without substances.
- Being irritable or angry when substances are removed.
- Being physically dependent on substances.
How Can First Responders Find Help?
First responders can get help through online counseling and a number of other resources. For those with mental health issues, cognitive behavioral therapy or talk therapy may be advised. Medications for depression, stress, and anxiety may also be part of the treatment. Those who are experiencing mental health issues could consider reaching out to an organization that deals specifically with first responders and the services they need.
If they’re worried about privacy or costs, first responders can find confidential services online and may be able to acquire in-person therapy through their health insurance providers. Some therapists also have sliding scale payment systems based on the amount of money an individual makes, so people might find more affordable payment options for therapy.
 Many firefighting, police, and EMS departments have their own internal health departments. Some may fear going to these therapeutic sessions because of repercussions, but they can be a good place to start for many.
Many firefighting, police, and EMS departments have their own internal health departments. Some may fear going to these therapeutic sessions because of repercussions, but they can be a good place to start for many.
Substance use disorder issues can be more complex because there is a physical component. Those who have serious substance use disorder issues should usually research physical care.
Inpatient services can give people the medical attention they need while they go through withdrawal, which can be medically dangerous. People can treat substance use disorder problems through inpatient and outpatient care, medication-assisted treatment to deal with withdrawal symptoms, counseling services, and other options. Resources such as Alcoholics Anonymous might be good options because they are an anonymous system of support.
Other than this, first responders can find help the same ways others can find assistance. Talk therapy, group therapy, and cognitive behavioral therapy are often advised.
If mental health problems such as stress and anxiety are severely impacting people, they might want to consider pursuing a different career or a less stressful area of their current career. Those with PTSD or other trauma-related issues may need time off to recover.
Some first responders may deal with their issues through medication, therapy, or a combination of both. In many situations, a combination of medication and therapy has been seen to be effective.
Because many first responders are afraid of damaging their career by pursuing help, they could consider joining a support group for first responders. A support group might help them figure out the best tactics to deal with their current issues. First responders often seek help anonymously at first, so many online services can be ideal. There are also many specific services that are designed for first responders and advocate groups for better mental health. Such resources acknowledge that first responders often have unique mental health challenges. They experience environments and scenarios that are dramatically different from what the average person. Some resources could include: An online therapy service, 7Cups allows people to chat with someone any time — twenty-four hours a day, seven days a week. While 7Cups is not a registered or certified therapy service, it can provide someone to talk to for those who feel alone or who want a sounding board for what they should do next. 7Cups should not be a replacement for actual therapy, but it can be a good place to get started, especially for those who don’t yet know what they want to do. This foundation is dedicated to helping first responders find crisis support and manage their mental health. It includes chat, text, and calling services as well as education. Those who are digging deeper into their mental health or substance use disorder issues may want to contact the AllClearFoundation to help them learn more about the issues that they face and find additional online and local resources that may be able to help them. Code Green Campaign is dedicated to spreading awareness of the mental health issues and substance use disorder issues first responders frequently face. The campaign provides in-depth resources, programs, and services for those who want to learn more about the risks that first responders generally experience, as well as the ways that they can manage and mitigate their symptoms. First Responder Center for Excellence (FRCE) provides free, online behavioral health services for first responders with the understanding that first responders experience unique issues that no one else does and operate in unique situations that others don’t. It helps people who have anxiety, depression, PTSD, and suicidal thoughts. FRCE also provides support for physical issues that can occur because of first responding environments, such as cancer. Designed specifically for first responders, ResponderStrong helps first responders connect with tips from others who have been in similar situations. The organization engages with first responders confidentially and anonymously so people don’t run the risk of having to expose themselves to their work too soon. Such assistance can give individuals the courage to deal with their mental health and substance use disorder issues on their own or visit a professional for assistance. Stepstone Connect provides online counseling services for first responders. It provides confidential, HIPAA-compliant sessions available for those who need to talk about their issues and receive therapeutic advice. People who are interested can request more information to determine whether the services are covered under insurance. Stepstone Connect can be a good first step for those who need to explore their issues.
Resources for First Responders
7Cups
AllClearFoundation
Code Green Campaign
First Responder Center for Excellence
ResponderStrong
Stepstone Connect
What’s Next?
First responders who are experiencing mental health or substance issues should try to secure help. Many jobs have programs for these purposes, but there are also anonymous, online services that can be used in the interim.
A first responder may also want to connect with their insurance company to learn if it has resources available for them. These resources could be free, operate on a sliding scale, or require a low copayment (copay).
Today, many insurance companies offer online or text-based therapy for first responders who are busy or work different shifts. Regardless of the help first responders seek, it’s important that they reach out to look for such assistance.
Sources
Medical disclaimer:
Sunshine Behavioral Health strives to help people who are facing substance abuse, addiction, mental health disorders, or a combination of these conditions. It does this by providing compassionate care and evidence-based content that addresses health, treatment, and recovery.
Licensed medical professionals review material we publish on our site. The material is not a substitute for qualified medical diagnoses, treatment, or advice. It should not be used to replace the suggestions of your personal physician or other health care professionals.







