Mental health issues for people in the Hispanic community take many different forms with cultural differences and systemic inequalities being key causes. Since mental health problems don’t just go away, being able and willing to take advantage of available resources can make all the difference in the world to your mental well-being and quality of life.
Mental health problems affect all types of people, regardless of who you are, where you come from, or how much money you have. And people from different walks of life tend to have different perspectives on mental health and mental health treatment.
Sometimes differing perspectives can prevent a person from getting the help they need when they need it. For Hispanic Americans, cultural differences and systemic inequalities in American society account for many of the mental health issues facing the Hispanic/Latino community.
Like physical ailments, mental health problems can severely limit your quality of life when left untreated. While it may seem easier to ignore mental and emotional distress, problems like these only get worse with time. The good news is there are Latino-friendly resources available for those who need them.
The Hispanic/Latino Community – A Changing Landscape
The Hispanic community in the U.S. encompasses a wide variety of ethnic groups, hailing from Mexico, Cuba, Puerto Rico, Spain, and Latin America. From a historic perspective, people of Mexican descent (and Native Americans) were the first to settle in what is now the United States. For centuries, the Hispanic population grew exponentially as groups from other Spanish-speaking countries immigrated to America.
These changes, coupled with the number of U.S.-born children of immigrant parents, account for today’s population of 60.6 million and also explains why Hispanics are the fastest-growing ethnic group in the country. Today, an estimated 45 percent of the Hispanic population is foreign-born while 31 percent are second-generation, U.S.-born. Consequently, many of the mental health issues facing the Hispanic/Latino community derive from the challenges foreign-born Latinos face versus the challenges U.S.-born Latinos face.
Mental Health Trends Within the Hispanic/Latino Community
The immigration experience and the process of integrating with a new society or culture can be stressful, to say the least. Day-in, day-out fears and concerns regarding one’s national identity and sense of belonging can easily give rise to mental health issues for people in the Hispanic community. As with minority populations, in general, ongoing discrimination and exclusion from employment and economic opportunities take a toll on a person’s ability to cope with daily life. These conditions place Hispanic immigrants and second-generation Latinos at greater risk of developing conditions like depression and PTSD.
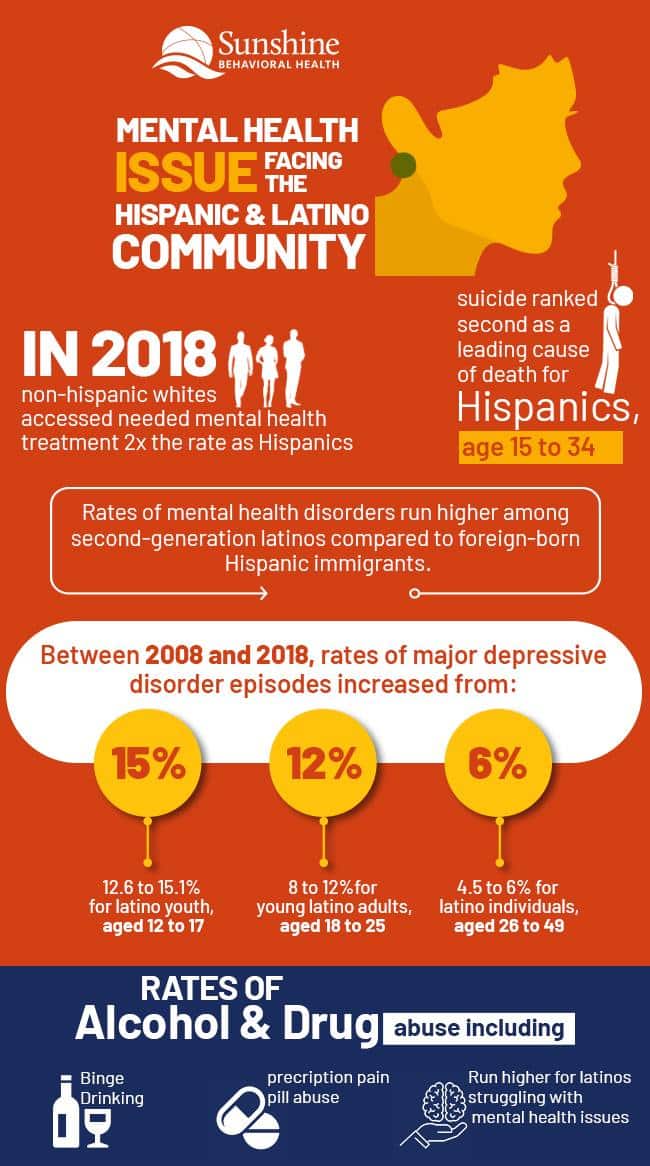
Here are a few statistics to consider:
- In 2018, non-Hispanic whites accessed needed mental health treatment at twice the rate as Hispanics.
- Suicide ranked second as a leading cause of death for Hispanics, aged 15 to 34.
- Hispanics living below the poverty line are more than twice as likely to report experiencing mental health problems compared to Hispanics living well above the poverty line.
- Rates of mental health disorders run higher among second-generation Latinos compared to foreign-born Hispanic immigrants.
- Between 2008 and 2018, rates of major depressive disorder episodes increased from:
- 12.6 to 15.1 percent for Latino youth, aged 12 to 17
- Eight to 12 percent for young Latino adults, aged 18 to 25
- 4.5 to six percent for Latino individuals aged 26 to 49
- Rates of alcohol and drug abuse, including binge drinking and prescription pain pill abuse, run higher for Latinos struggling with mental health issues
Barriers to Mental Health Care facing the Hispanic Community
Cultural Barriers
Every culture harbors its own unique perspectives and attitudes regarding the body and the mind. Sometimes, differences between cultures can create misunderstandings that become a force unto themselves. In American culture, doctors and therapists typically view mental illness as a disease- or body-based condition caused by heredity, brain chemical imbalances, or chemical imbalances caused by childhood trauma. In the case of an American therapist treating a Latino patient, this perspective doesn’t sit well with the patient’s cultural beliefs.
A 2010 comparative study appearing in Transcult Psychiatry set out to determine how different cultural perspectives regarding mental illness impact the therapist-patient relationship. Study participants included a total of 25 Latinos, African Americans, and European Americans from the inner-city region of Hartford, Connecticut. All 25 participants also struggled with severe mental illnesses. Results from the study showed the Latino and African American participants were resistant to the idea that their mental health issues stemmed from a physical problem while the European Americans had little to no problem with this perspective. Overall, the Latino and African American participants were much more critical of mental health care approaches than their European American counterparts.
Doctors not trained or aware of mental health issues in the Latino community also face the risk of misdiagnosing patient-reported symptoms. For example, a Latino patient experiencing depression may use words like tiredness or feeling nervous while avoiding words like sadness or feeling discontent, when questioned by a doctor. In turn, the doctor may misread symptoms like tiredness and nervousness as hypoglycemia (low blood sugar) or something else, even though they’re also symptoms of depression.
Also, Hispanic culture tends to adhere to distinct gender roles for men and women. Men are expected to be strong, self-sufficient providers for their families while women are charged with caring for the home and family. Since these roles hold a high priority, they leave little room for individuals to attend to personal, self-care needs, like mental health.
Religion-Based Biases
Religion plays an important, supporting role in Hispanic culture. Faith-based communities can offer considerable support during difficult times for any society or culture. The only drawbacks arise when skewed perceptions that disregard the benefits of professional healthcare come into the picture. For these reasons, turning to religion-based supports instead of getting needed treatment help may be one of the things that contribute to ongoing mental health issues in the Hispanic community.
A 2019 study published in Hispanic Health Care International, entitled “Intersection of Cultural and Religious Beliefs About Mental Health: Latinos in the Faith-Based Setting” set out to identify beliefs towards mental illness within Latino faith-based communities. Results from the study showed community-based social norms and perceptions had considerable influence on how participants viewed mental illness. These perspectives also dictated how they coped with mental and emotional distress.
For the majority of families interviewed, it was common practice to deny signs of depression unless symptoms greatly interfered with their ability to manage daily life affairs. Participants rather viewed lapses in faith, not praying, demonic forces, and the sins of their parents as causes for mental and emotional distress. In turn, participants reported coping with mental health issues by using their faith in God and prayer as protections. While faith can be a powerful force, Hispanic social norms and perceptions about mental illness are factors that incite mental health issues in the Latino community.
Language Barriers
 While the Latino population consists of more than a few ethnicities, all of them hail from Spanish-speaking countries. Since English is the national language in the United States, for some Hispanic households, language differences become one of the mental health issues facing the Hispanic/Latino community. Results from a 2018 Census survey show approximately 13.5 percent or 41 million Latinos speak Spanish at home. Of this number, 23.1 million respondents report being able to speak English “very well” while 6.8 million respondents report speaking “well.”
While the Latino population consists of more than a few ethnicities, all of them hail from Spanish-speaking countries. Since English is the national language in the United States, for some Hispanic households, language differences become one of the mental health issues facing the Hispanic/Latino community. Results from a 2018 Census survey show approximately 13.5 percent or 41 million Latinos speak Spanish at home. Of this number, 23.1 million respondents report being able to speak English “very well” while 6.8 million respondents report speaking “well.”
In effect, language differences can place first-generation Hispanic households at a considerable disadvantage. Households that speak mainly Spanish are twice as likely to become isolated in terms of not being able to integrate with society at large. Also, this state of isolation can continue on into the second and third generations.
Within the context of mental health treatment, language differences make it difficult to get the help you need when medical professionals don’t speak Spanish. This is especially true when trying to describe thoughts, emotions, and fears to a therapist or counselor. In 2016, only 5.5 percent of psychologists reported being able to provide services for Spanish-speaking patients. This lack of diversity within the mental health field combined with cultural language gaps are two of the biggest mental health issues for people in the Hispanic community.
Stigmas
Stigmas regarding psychological problems, in general, are another driver of mental health issues facing the Latino community. Not unlike other ethnic minority groups, privacy regarding personal matters is the norm in the Hispanic community. This means talking about one’s problems is akin to “airing your dirty laundry in public.” From this frame of mind, it’s easy to see how someone struggling with emotional issues would feel shameful and afraid to talk about them.
Talk-therapies or “talk-based” treatment approaches require you to open up about personal issues (many of which may be uncomfortable to discuss). Since talking about these types of problems goes against cultural norms, Hispanics are less likely to seek out treatment help. In effect, a lack of understanding and knowledge about mental health and mental health treatment creates prime conditions for stigmas to develop. Likewise, if a person doesn’t recognize symptoms of mental illness when they appear, he or she is not likely to take them seriously.
Access to Mental Health Resources
Mental health problems impact people of all kinds, regardless of ethnicity or socioeconomic status. However, the rate at which different groups use available treatment services varies considerably. The mental health issues facing the Latino community can have ripple effects that not only affect a person’s willingness to seek treatment but also limit his or her ability to access mental health resources. Cultural biases surrounding mental health leaves individuals with little to no knowledge of how to go about getting treatment help or where to find it.
Health Insurance
With healthcare costs on the rise, having adequate insurance coverage not only makes getting treatment affordable but possible. An estimated 19 percent of Latinos had no form of health insurance in 2018. In that same year, a whopping 56.8 percent of Latinos (aged 18 to 25 years) struggling with serious mental health problems did not receive treatment.
Part of the reason for this has to do with citizenship status concerns and fear of deportation. Present-day health insurance laws (the Affordable Care Act) make provisions for health insurance coverage for children regardless of citizenship status. Unfortunately, immigrant parents without legal documentation don’t take advantage of this resource due to deportation fears. These concerns combined with the stigmas that surround mental illness greatly contribute to the mental health issues in the Hispanic community.
Substance Use Disorder Issues
When substance use disorder issues enter the picture, seeing mental health problems becomes that much harder. Mental health issues and substance use disorder tend to attract one another, and when combined, can quickly snowball out of control. In 2018, nearly 90 percent of Latinos with substance use disorders did not receive treatment.
Untreated drug and alcohol problems only add fuel to the fire when conditions like depression, PTSD, and anxiety are at work. The truth of the matter is no amount of counseling or therapy can help when substance use disorder problems persist. This means, getting needed rehab treatment help has to be the first step towards reclaiming your mental health.
Hispanic/Latino-Friendly Mental Health Resources
Anxiety and Depression Association of America
Anxiety and depression-based conditions rank first and second as the most commonly experienced mental disorders affecting Americans, today. An estimated one out of every six adults will experience depression at some point in their lives while approximately half of those diagnosed with depression will also have an anxiety disorder. Not surprisingly, anxiety and depression are mental health issues in the Latino community.
The Anxiety and Depression Association of America or ADAA offers a safe place for people to support one another and talk to people who understand. They are a non-profit organization that serves over 11 million visitors a year. Most of the resources offered are free, some of which include:
- Podcasts
- Webinars
- Support groups
- Videos
- Blog posts
ADAA also has both English- and Spanish-speaking peer-to-peer support group forums where you can participate and interact, anonymously:
Therapy for Latinx
Therapy for Latinx acknowledges the stigma surrounding mental health problems and how difficult it is to find a therapist that understands the Hispanic culture. This site provides a way to search for Latino therapists that you can meet with using telehealth or person-to-person video sessions. With their search bar, you can look for a therapist by:
- Name
- Specialty
- Type of health insurance covered
- Therapist by gender
- Payment type
As long as a therapist is licensed in your state, they can work with you.
National Suicide Prevention Lifeline
1a800a273aTALK (8255)
When mental and emotional problems go untreated, things can boil over to a point of desperation. When this happens, having someone to listen and talk with can mean the difference between working through a traumatic, temporary situation and doing something that can’t be undone. The National Suicide Prevention Lifeline offers free and confidential emotional support for anyone who’s in emotional distress or considering suicide.
Their helpline, which is called Lifeline, is available 24 hours a day, seven days a week. Lifeline consists of a national network of more than 180 local crisis centers. Their crisis centers will not only help you through times of crisis but refer you to resources in your community, many of which offer free services. Lifeline also offers its service for Spanish-speaking callers along with a resource page.
La Familia
San Francisco Bay Area
First founded in the 1980s, La Familia has a solid history of providing mental health and community support services that meet the needs of individuals and families in the San Francisco Bay area. La Familia understands the mental health issues facing the Latino community and fights to bring about the systems and services that can improve the quality of life for all community members.
Along with counseling and case management services, La Familia runs several crisis hotlines that answer calls 24 hours a day, seven days a week. Here’s a partial list of their available crisis lines:
- Domestic violence
- Runaways
- Eating disorders
- Youth crisis hotlines
- Dating abuse
- Suicide
- Veterans assistance
- Addiction recovery
SAMHSA’s National Helpline
1a800a662aHELP (4357)
The SAMHSA National Helpline offers free, confidential, mental health, and substance use disorder treatment referral services. SAMHSA provides both English- and Spanish-speaking phone assistance at any time of the day or night, even holidays. Phone representatives can refer you to local drug and alcohol treatment facilities, support groups, and other community-based organizations. You can also order free mental health information resources online and over the phone. Whether you have health insurance or not, SAMHSA can help you find affordable treatment help.
More Resources to Check Out
Multicultural Mental Health Resource Centre, Mental Health Information and Resources in Spanish
Mental Health America, Peer Supports
Anxiety and Depression Association of America, Online Screening Tools
Postpartum Support International, PSI Helpline (English and Spanish)
Sources
Medical disclaimer:
Sunshine Behavioral Health strives to help people who are facing substance abuse, addiction, mental health disorders, or a combination of these conditions. It does this by providing compassionate care and evidence-based content that addresses health, treatment, and recovery.
Licensed medical professionals review material we publish on our site. The material is not a substitute for qualified medical diagnoses, treatment, or advice. It should not be used to replace the suggestions of your personal physician or other health care professionals.